Outpatient facilities have become the darlings of the healthcare construction sector in recent years. By even the most conservative measure, spending on outpatient construction is expected to grow anywhere from 20-30% in the next decade.
“In the early 1990s, outpatient care accounted for only 10 to 15% of hospital revenue; today, it’s closer to 60%,” says Patrick Duke, Senior Vice President with KLMK Group, Richmond, Va. “It’s a shift that’s been happening across the board, sweeping along academic medical centers, community hospitals, for-profit chains, and not-for-profit providers alike,” says Duke, a Building Design+Construction “40 Under 40” honoree. “And it’s showing no sign of slowing, especially with advancements in care and changing reimbursement patterns.”
This shift in service modes should not be surprising. Outpatient facilities typically allow healthcare organizations and physician groups to deliver care at lower cost than can be done in inpatient environments. They are generally less expensive to design, build, operate, and maintain, which translates to higher profits for their owners. And with the Affordable Care Act on the horizon, demand for outpatient care facilities is likely to accelerate.
What healthcare clients are demanding from Building Teams
1. EXPECT DEMAND for easily reconfigurable spaces in outpatient facilities to be on the rise.
2. BE PREPARED to rethink the conventional wisdom about underfloor air systems in healthcare facilities.
3. LOOK FORWARD to heightened scrutiny of facility quality and operational performance.
4. ANTICIPATE greater pressure from clients for you to deliver ‘affordable elegance.’
5. WATCH FOR healthcare providers to put you on a ‘Lean’ diet.
However, these kinds of projects are becoming increasingly difficult to execute, as healthcare clients see outpatient environments as a means not only to deliver better patient outcomes and experiences, but also as a way to provide flexibility to meet their own rapidly changing organizational needs and strategies.
Building Design+Construction combed the healthcare design and construction sector to evaluate the latest developments in outpatient facility designs. Here are five radical trends to watch.
1. Expect demand for easily reconfigurable spaces in outpatient facilities to be on the rise.

At the Spectrum Health ambulatory center, exam and procedure rooms are located at the center of the plan, rather than at the perimeter, to create a more reconfigurable environment. Interior exam rooms receive daylight through clerestory windows. Designers from Integrated Architecture used mockups to test room configurations. Photo: Justin Maconochie
Like most large healthcare providers, Spectrum Health System. a seven-hospital nonprofit system in Grand Rapids, Mich., is constantly struggling to stay ahead of changing conditions in the healthcare field. With more than two-dozen inpatient and outpatient locations throughout Michigan, having to deal with this moving target puts a huge burden on Spectrum’s facilities.
On average, Spectrum makes a major renovation to its spaces every four years. “In some cases, they’re touching spaces every two years,” says Michael Corby, FAIA, LEED AP, Executive Vice President with Integrated Architecture, Grand Rapids, who has worked on multiple projects for Spectrum. “It is extremely costly, as you can imagine.”
To reduce both costs and the noise, dust, and disruption associated with renovation work, while simultaneously enhancing operational efficiency, work environments, and patient experience, Spectrum Health commissioned Integrated Architecture to develop a highly flexible, reconfigurable outpatient facility model.
The designers tested a number of physical mockups to get the optimal configuration, which turned out to be a 9x12-foot patient exam room. “Once we got the exam room piece resolved, we started to build on that,” says Corby.
All other spaces became increments of the exam room module: a procedure room becomes one-and-a-half times the size of an exam room; a utility room becomes half the size of an exam room—“so they can replace an exam room with, let’s say, two utility room modules,” says Corby.
Corby says the team put the design scheme to the test halfway into the construction documentation process, when Spectrum decided to shift its care groups around. “Imagine that, halfway into the planning, the client says to you, ‘We’re going to move primary care up here and subspecialists over there,’ it would have been disastrous under a traditional planning process,” he says. “But because of the modularity, it took us all of 60 minutes to redo the floor plan.”
The resulting design scheme was first applied at Spectrum Health Medical Group’s new ambulatory center in Holland, Mich., and is currently being replicated at several other outpatient centers in Spectrum’s network. The 58,000-sf facility follows a consolidated delivery model, where both primary-care providers and subspecialists are housed under a single roof. “This has been done before, but what is unusual is the fact that they wanted the mix to not be limited by the facility,” says Corby.
To achieve the kind of flexibility of spatial use that the client wanted, Integrated Architecture had to depart from more traditional outpatient facility plans. For instance, the exam rooms are located in the central core of the facility instead of at the perimeter. With its open-plan configuration, the facility incorporates underlying modularity that allows patient rooms, workspaces, conference rooms, and other spaces to change in function, location, and dimension as needed, without the need for intense renovation.

The floor plan for Spectrum’s Holland, Mich., facility was organized around the dimensions of the exam rooms (green), which were optimized at 9X12 feet using physical mockups. The resulting 30-foot-wide bays responded to the unit size of the exam rooms. All other rooms, including procedure rooms (large green) and utility spaces (blue), became multiples of the exam room module.
CLICK TO ENLARGE PLAN - FIRST LEVEL
CLICK TO ENLARGE PLAN - SECOND LEVEL
[pagebreak]
2. Be prepared to rethink the conventional wisdom about underfloor air systems in healthcare facilities.

Underfloor air distribution is one of the design innovations at the new Spectrum Health Medical Group’s ambulatory center, in Holland, Mich. The UFAD scheme reduces energy consumption and allows the spaces to be reconfigured without dramatic renovation costs. Photo: Justin Maconochie
How do you make a roomful of healthcare design and infection control experts utter a collective gasp? Simple. Just mention “healthcare” and “UFAD” in the same sentence.
That’s what happened when Corby presented underfloor air distribution for the new Spectrum Health facility to a group of healthcare professionals last fall. “For a lot of people, especially those who are involved with infection control, it scares them,” says Corby.
He insists that UFAD is safe for outpatient care facilities like the one in Holland, Mich. “Spectrum’s infection control experts checked it out and found no inherent issues from an infection control standpoint,” he says. “It’s actually healthier, because the air is coming to the occupants in its freshest state. You’re not mixing the stale air that’s rising through the ductwork.”
However, Alan Kranzo, Spectrum’s Director of Facility Planning and Operations, cautions that the technology may not be appropriate for every outpatient facility. “The Spectrum facility was an ambulatory patient visit environment, where they’re just doing patient exams,” he says. “We would never consider UFAD in an operating room, where procedures are being done.”
In pitching the idea of using UFAD to Spectrum management, Corby and his team analyzed the average cost and operational impact of recent renovations at the organization’s other facilities. “We showed them that, had these facilities had UFAD, they would have saved 30% on average of the cost of the renovation, because they would not have had to core through floors, shut down operations, and affect the surrounding areas,” he says.
In fact, underfloor air distribution (in combination with Spectrum’s modular facility plan) has enabled the organization to change out spaces much faster and at lower cost, without dramatically affecting daily operations.
The technology pencils out on the initial cost side, too. The entire Spectrum facility uses UFAD, at a first cost of $6-7/sf. But when the upfront savings on mechanical system components (less ductwork, smaller fans, etc.) is factored in, the investment is a wash, says Corby. On top of that, the project’s energy models show that UFAD will deliver anywhere from 20 to 30% savings in ongoing energy costs.
Corby expects to see more healthcare organizations give UFAD a closer look as they search for ways to create more flexible and adaptable outpatient spaces. “I think it’s revolutionary as it is related to healthcare,” says Corby, who has done four UFAD applications for healthcare clients.
[pagebreak]
3. Look forward to heightened scrutiny of facility quality and operational performance.

To ensure all its facilities meet benchmark levels of quality for patient experience and operational and facility performance, Spectrum Health’s facilities team developed a prescriptive-based facility assessment tool. Using the tool, they score their facilities on everything from the quality of the furnishings to the distance a patient walks from the parking lot. Photo: Justin Maconochie
No other building sector is more keenly focused on the performance and continual assessment and improvement of its buildings than healthcare. This emphasis on quality will be further emphasized with the coming implementation of the Affordable Care Act, which is expected to place heavy pressure on healthcare providers to take a cleaver, not a surgical knife, to operating costs. That means outpatient care centers will have to deliver more care—and higher-quality care—at less cost.
“There’s no doubt that physician groups are more closely analyzing how to turn over the outpatient exam rooms,” says Brian McFarlane, AIA, Principal in HKS’s Healthcare Group, in Dallas, who leads the firm’s healthcare business development. Already, outpatient clients are using kiosks for check-ins, and they’re administering injections outside of exam rooms to eliminate bottlenecks in patient flow and speed up turnover of exam rooms.
“Less time in exam rooms may mean fewer rooms required or less square footage, which means lower rent for each physician, operational savings, and increased revenue. It’s real money,” he says. “The perfect situation is when a patient parks the car, walks in the door, quickly checks in via kiosk or in person, and goes directly to an exam room.”
What, then, does this heightened emphasis on quality and proof of performance mean for Building Teams working on outpatient facilities?
You can expect greater scrutiny of the quality of your work, especially as it pertains to the efficiency, flexibility, and profitability—not to mention the patient experience—of outpatient facilities. Physical mockups and computer simulations are great, but the end product must perform up to expectations and be able to flex as the client’s needs change.
To help assess the design and performance of its buildings, Spectrum Health’s facilities team, assisted by Integrated Architecture’s Kranzo, created a prescriptive-based facility assessment tool that scores everything from the patient’s experience as they approach and enter the facility, to the quality of the work environment for physicians and staff, to the performance of both the operations and the building itself.
Typical questions: Is the reception area clearly visible immediately upon entering the building? Are there landscaped areas at or near the entry? Are there preferred views from and natural light in 75% of the hospitality area? How visible is the exterior signage from the primary access road? How effective are the primary landmark elements in wayfinding? What is the quality of the furnishings?
Kranzo says his team created the scorecard in an effort to develop facilities that are as balanced as possible across the multiple categories. The prescriptive criteria were developed based on evaluations of three recently renovated ambulatory centers, and were used to inform the design of the new Holland facility.
“It really came out of us trying to measure the quality of a design as part of our final approval process of a construction document,” says Kranzo. “We’re not going to focus just on the facility performance. We’re going to rate operational efficiency as well as the experiential side for the patients and staff.”
Before Kranzo signs off on a CD for new construction or a renovation, a design must achieve a certain score level. Most elements are scored using a plus-three, minus-three system, allowing for gradations and some interpretation.
The goal, says Kranzo, is to “have zeros across the board.” This ensures that no single element is drastically underdesigned or overdesigned. “We found that some facilities go overboard in certain areas, such as finishes being well beyond what we need,” he says. “This standard works to balance everything. That then feeds how we utilize our capital and budget on a given project.”

In a somewhat unusual move for a healthcare facility, Spectrum Health placed the physician and administrative workspaces along the perimeter of the structure, thus providing staff with the best daylight and views for completing medical documentation and reports. Photo: Justin Maconochie
[pagebreak]
4. Anticipate greater pressure from clients for you to deliver ‘affordable elegance.’

To keep costs to a minimum and deliver what the client termed “affordable elegance,” the Building Team for the Everett Clinic’s new Smokey Point (Wash.) Medical Center—ZGF Architects (designer), Coughlin Porter Lundeen (structural engineer), Affiliated Engineers (MEP engineer), and J.R. Abbott Construction (GC)—used tilt-up concrete for the shell of the structure. The move saved an estimated $160,000 in construction and material costs. Photo: Benjamin Benschneider
As if delivering highly efficient, flexible, and patient-focused facilities wasn’t difficult enough, Building Teams can look forward to having clients up the ante on exterior and interior architecture schemes. As healthcare institutions and physician groups compete for outpatient business, they’re increasingly leaning on their facilities to help attract and retain both patients and employees, while keeping budgets tight for designing and constructing outpatient facilities.
To deliver world-class facilities on constrained budgets, Building Teams are getting creative in the selection of materials, finishes, and construction methods.
Take, for example, the Everett Clinic’s new Smokey Point (Wash.) Medical Center. The two-story, 60,000-sf facility was built for around $200/sf—“a budget that is unheard of for this building type,” says Anita Rossen, Senior Healthcare Interior Designer with ZGF Architects, the project’s architect. “Because they are physician-owned, cost was a huge factor. The term their CEO used throughout the design and planning process was ‘affordable elegance.’”
Rossen says the Building Team, which included contractor J.R. Abbott Construction, Seattle, MEP engineer Affiliated Engineers, Chicago, and structural engineer Coughlin Porter Lundeen, Seattle, identified dozens of alternative design and construction approaches and materials and finishes that resulted in more than $350,000 in upfront savings.
The most startling of these was the use of tilt-up concrete construction for the shell of the structure—a construction method that is more popularly associated with big-box stores and warehouses than modern healthcare facilities. The move saved an estimated $160,000 in construction and material costs, according to Michael Sloane, LEED GA, Project Engineer with J.R. Abbott.
“Tilt-panel construction reduced the number of trades involved in the exterior skin, which reduced the number of costly handoffs or transitions,” says Sloane. “It also reduced the number of layers on the exterior from five to two.” That means no metal studs, sheathing, or vapor barrier; just the concrete panel and insulation. Sloane says going with tilt-up saved $8/sf over traditional masonry wall construction.
But how to break up the massing so that the building wouldn’t look like a boxy warehouse? That was the problem before the design team. “We wanted it to feel extremely inviting—a healthcare facility that you would actually want to go to for care,” says Rossen.
To break up the box, the team varied roofline angles and introduced glass curtain wall, storefront windows, wood and metal accents, and vertical reveals in the concrete panels.
To create the “inviting” interior, Rossen says the team brought the concrete panel reveals and exposed wood elements inside to complete the custom, modern look.
Several other “affordable elegance” measures were employed on the project, including the use of mostly off-the-shelf floor tile that was installed in a staggered pattern in the main entry area and stairway for a custom aesthetic; wood-pattern vinyl flooring in lieu of more costly flooring products; and naturally finished local western red cedar instead of hardwoods like ipe or teak.
These are the kinds of low-cost, value-added solutions Building Teams are going to have to provide if they expect to succeed in the outpatient facility market.

To break up the massing of the tilt-up concrete box, the design team incorporated wood and metal accents and vertical reveals in the concrete panels. Using tilt-up cut the number of layers in the building envelope from five to two, thereby saving $8/sf over traditional masonry construction. Photo: Benjamin Benschneider
[pagebreak]
5. Watch for healthcare providers to put you on a ‘Lean’ diet.

Exposed wood elements were also used in the interior of the Everett Clinic project to create a warm, modern design aesthetic. Photo: Benjamin Benschneider
A growing number of healthcare organizations are turning to so-called Lean principles as a means to increase efficiencies and reduce cost in their day-to-day operations. The core tenets of Lean dictate that organizations identify and remove all waste in their products, services, and processes––everything from lengthy waiting times for patients, to excessive costs for supplies and equipment, to unnecessarily long walking distances for clinicians and staff. Implementing Lean operations can involve mapping and evaluating thousands, if not hundreds of thousands, of processes for continual improvement.
Because the design, construction, operation, and maintenance of facilities all play a major role in these Lean efforts, healthcare clients will be looking to their Building Teams to take part in their Lean efforts on new construction projects. This requires a deeper level of team collaboration much earlier in the planning process than some AEC firms may be accustomed to. In some cases, it may be the client’s first foray into applying Lean principles toward facilities construction, thus adding yet another level of difficultly for you to deal with.
“We’re seeing that across the board for projects in our area,” says Rossen. “Healthcare groups that have implemented Lean in their operations are now using it to drive the design and construction on their new facilities. And we’re at that moment in history where most clients haven’t done this before for a new building.”
As a result, clients are relying on their AEC firms to facilitate the Lean process for the project, so be prepared to know your stuff. This may include facilitating integrated design events and building full-scale mockups to get input not only from your Building Team partners but also from patients, staff, and facility operations professionals. And if the client is not fully committed to Lean, expect a rocky road, says Rossen.
“We get RFPs all the time that ask about how much Lean experience we have and if we can facilitate the process,” she says. “You want the clients to own the process and be fully committed to it.”
There is also the potential for conflict between Lean and evidence-based design. “Lean requires a highly flexible environment,” says Rossen. “So how do you create a high degree of flexibility while maintaining the healing qualities of evidence-based design?”
For example, applying Lean principles in an outpatient clinic could mean having no cabinets on the wall––all exam-room supplies would have to be housed in a mobile cart, and all clinician tools would be out in the open. Such an arrangement could be considered a violation of EBD principles.
To solve this conundrum, the Building Team on the Smokey Point Medical Center specified integrated systems furniture with a mix of demountable partitions and tables and chairs that makes it easy to reconfigure exam room spaces.
The same approach was applied in the main lobby, where the front desk and check-in areas use demountable partitions and systems furniture instead of permanent construction. “The trick is to make it not look like a workstation that was designed for an office building,” says Rossen.
Related Stories
Urban Planning | Apr 12, 2023
Watch: Trends in urban design for 2023, with James Corner Field Operations
Isabel Castilla, a Principal Designer with the landscape architecture firm James Corner Field Operations, discusses recent changes in clients' priorities about urban design, with a focus on her firm's recent projects.
3D Printing | Apr 11, 2023
University of Michigan’s DART Laboratory unveils Shell Wall—a concrete wall that’s lightweight and freeform 3D printed
The University of Michigan’s DART Laboratory has unveiled a new product called Shell Wall—which the organization describes as the first lightweight, freeform 3D printed and structurally reinforced concrete wall. The innovative product leverages DART Laboratory’s research and development on the use of 3D-printing technology to build structures that require less concrete.
Market Data | Apr 11, 2023
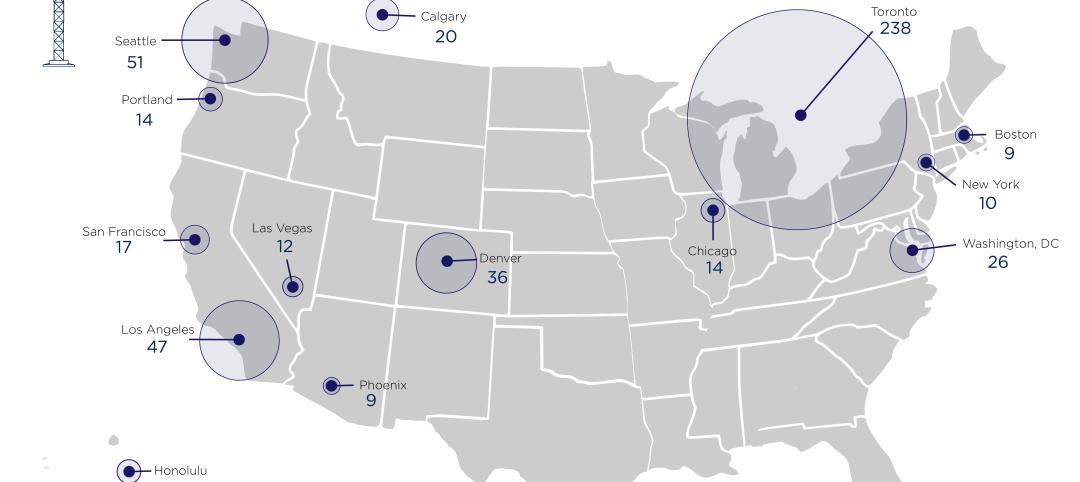
Construction crane count reaches all-time high in Q1 2023
Toronto, Seattle, Los Angeles, and Denver top the list of U.S/Canadian cities with the greatest number of fixed cranes on construction sites, according to Rider Levett Bucknall's RLB Crane Index for North America for Q1 2023.
University Buildings | Apr 11, 2023
Supersizing higher education: Tracking the rise of mega buildings on university campuses
Mega buildings on higher education campuses aren’t unusual. But what has been different lately is the sheer number of supersized projects that have been in the works over the last 12–15 months.
Architects | Apr 10, 2023
Bill Hellmuth, FAIA, Chairman and CEO of HOK, dies at 69
William (Bill) Hellmuth, FAIA, the Chairman and CEO of HOK, passed away on April 6, 2023, after a long illness. Hellmuth designed dozens of award-winning buildings across the globe, including the Abu Dhabi National Oil Company Headquarters and the U.S. Embassy in Nairobi.
Contractors | Apr 10, 2023
What makes prefabrication work? Factors every construction project should consider
There are many factors requiring careful consideration when determining whether a project is a good fit for prefabrication. JE Dunn’s Brian Burkett breaks down the most important considerations.
Mixed-Use | Apr 7, 2023
New Nashville mixed-use high-rise features curved, stepped massing and wellness focus
Construction recently started on 5 City Blvd, a new 15-story office and mixed-use building in Nashville, Tenn. Located on a uniquely shaped site, the 730,000-sf structure features curved, stepped massing and amenities with a focus on wellness.
Smart Buildings | Apr 7, 2023
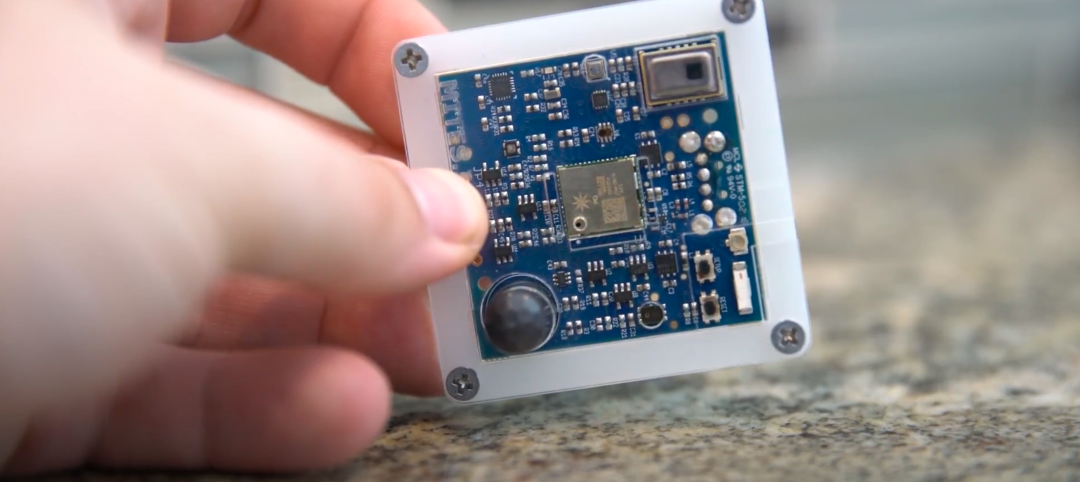
Carnegie Mellon University's research on advanced building sensors provokes heated controversy
A research project to test next-generation building sensors at Carnegie Mellon University provoked intense debate over the privacy implications of widespread deployment of the devices in a new 90,000-sf building. The light-switch-size devices, capable of measuring 12 types of data including motion and sound, were mounted in more than 300 locations throughout the building.
Affordable Housing | Apr 7, 2023
Florida’s affordable housing law expected to fuel multifamily residential projects
Florida Gov. Ron DeSantis recently signed into law affordable housing legislation that includes $711 million for housing programs and tax breaks for developers. The new law will supersede local governments’ zoning, density, and height requirements.
Energy Efficiency | Apr 7, 2023
Department of Energy makes $1 billion available for states, local governments to upgrade building codes
The U.S. Department of Energy is offering funding to help state and local governments upgrade their building codes to boost energy efficiency. The funding will support improved building codes that reduce carbon emissions and improve energy efficiency, according to DOE.