The era of unbearably long waits in cramped, impersonal emergency rooms may be drawing to a close.
In response to the far-reaching requirements of the Affordable Care Act, cutthroat competition from a flood of new healthcare providers, and the demands of an increasingly discerning patient population, hospital systems are reformulating their emergency departments into more welcoming, more efficient environments.
Because the ED is often the gateway to admissions, healthcare systems are reimagining their emergency facilities with an eye toward strengthening relationships with individual patients and the communities they serve.
This shift in perspective comes as demand for ED services across the U.S. faces rapid growth. Nearly half of emergency physicians responding to a recent poll by the American College of Emergency Physicians reported a rise in emergency visits since
7 FACTORS DEFINING THE NEW ED
1. Heightened emphasis on improving patient outcomes and quality of care.
2. Use of Lean concepts to optimize operational efficiencies.
3. Super-flexibility for quick expansion.
4. Deeper—much deeper—integration of technology.
5. Greater outreach to the community.
6. Enhanced preparation for catastrophic incidents.
7. Rise of the freestanding emergency center.
January 1, 2014. Close to 90% said they expected emergency visits to increase over the next three years; more than three-fourths (77%) said their EDs are not adequately prepared for such an increase in volume.
In light of these projections, Building Design+Construction asked a cross section of healthcare experts to discuss the factors that are influencing the design, construction, and operation of today’s ED projects. Following is a summary of their insights.
1. Heightened emphasis on improving patient outcomes and quality of care.
Patient care is always the top priority of hospitals and their emergency departments, but the Affordable Care Act raises the stakes through “pay for performance” provisions that reward healthcare providers for delivering higher quality care and penalize those that fall short. Under the Hospital Value-Based Purchasing Program, Medicare pays hospitals according to how well they perform on a set of clinical quality measures, such as readmission rates. Hospitals with higher-than-expected readmissions have already been penalized millions of dollars by Medicare.
“If an ED is going to be reimbursed on the quality of care, rather than volume, wait times have to be reduced and outcomes have to be improved,” says Andrew Quirk, National Director of the Healthcare Center of Excellence at Skanska USA Building. “Quality of care is the major focus of today’s ED projects. They’re all rooted in the idea of what’s the most efficient way that we can deliver healthcare.”
One response to patient privacy and infection control concerns has been an increase in private rooms for higher-acuity patients, not just in the hospital acute-care setting but within the ED as well.
At a new ED under construction at Yuma (Ariz.) Regional Medical Center, all but four of the 69 treatment rooms are private. The expanded facility will further serve as a unifying structure that will connect the hospital’s existing bed towers and its Women and Children Services Center.
“The current ED was built in the early ’90s to service about half as many patients as it currently sees,” says Kurt Nyberg, Project Director, McCarthy Building Companies.
2. Use of Lean concepts to optimize operational efficiencies.
“Because many EDs are overwhelmed, they are trying to find ways to do more with less,” says David Vincent, AIA, ACHA, LEED AP, Associate Principal and Director of Team ED at healthcare design giant HKS. Hospitals want to increase the productivity of their ED operations so they can get more patients through the system as effectively and efficiently as possible, he says.
One route hospitals are taking to maximize efficiency and throughput in their ED operations is to use Lean principles and methodologies. “Lean is a tool to help the ED reduce lengths of stay, improve the quality of work, lower costs, and improve patient and staff satisfaction,” says Marvina Williams, RN, Healthcare Clinical Operations Expert at Perkins+Will.
 A pediatric waiting room at the University Health System ED in San Antonio, Texas, provides a child-friendly environment for pediatric patients and their families. Designed by Perkins+Will, the colorful play area is separated from treatment areas serving adult patients. Photo: Charles Davis Smith, AIA
A pediatric waiting room at the University Health System ED in San Antonio, Texas, provides a child-friendly environment for pediatric patients and their families. Designed by Perkins+Will, the colorful play area is separated from treatment areas serving adult patients. Photo: Charles Davis Smith, AIA
A registered nurse and Lean black belt, Williams guides hospital EDs through the implementation of observation studies, data analysis, and operational modeling. The data can help determine the ideal size and configuration of ED facilities for optimal performance. She points to a recent study that used simulation modeling to show that the planned ED facility was larger than necessary, and that a number of rooms could be eliminated, thereby saving initial construction costs and long-term maintenance costs.
The study also identified opportunities to improve front-end operations and patient flow through the creation of a split-flow rapid medical evaluation unit. In split-flow triage, a medical team evaluates patients when they arrive and places higher-acuity patients in regular treatment rooms, while less serious conditions are treated in space-efficient, fast-track environments. “Time from door to doctor was significantly reduced, and the main ED beds were reserved for more-acute patients,” says Williams.
3. Super-flexibility for quick expansion.
EDs need to expand and contract quickly to accommodate wide swings in patient volumes. They must be inherently flexible, especially when they have to take on unexpectedly high patient loads—after a major highway accident, for example.
Designers at HKS have been exploring alternatives to traditional circular ballroom or individual pod configurations, which can be hard to adapt without wasting space or overburdening staff due to the design’s inherent inflexibility.
A linear concept, by contrast, organizes treatment rooms into two parallel rows, with a staff work area in between. Rooms have a second entry point from a perimeter corridor for access by patients and visitors.
 Since introducing a Rapid Medical Evaluation module in its ED, MidState Medical Center in Hartford, Conn., has significantly cut patient wait times. The module allows for rapid assessment and treatment of patients and reserves emergent beds for more-acute patients. Perkins+Will used Lean concepts to design future-state process maps and floor plans. Photo: Eduard Hueber/Archphoto
Since introducing a Rapid Medical Evaluation module in its ED, MidState Medical Center in Hartford, Conn., has significantly cut patient wait times. The module allows for rapid assessment and treatment of patients and reserves emergent beds for more-acute patients. Perkins+Will used Lean concepts to design future-state process maps and floor plans. Photo: Eduard Hueber/Archphoto
“The advantage of the linear topology is that if you want to expand it—even by just one bed—you could clip it on without changing any part of the ED design,” says Jim Lennon, AIA, ACHA, LEED AP, Associate Principal, HKS
EDs also must be equipped to deal effectively with the wide range of medical problems that patients present. This has led to the rise of universal, acuity-adaptable, same-handed treatment rooms.
“In the past, we used to designate treatment points, such as a suture room or a pediatric room,” says Patti Meszaros, Director of Facility Planning at Mercy Health, in Cincinnati. “Now we’ve become far more flexible with our treatment points. One exam room treats all.”
4. Deeper—much deeper—integration of technology.
Technology continues to permeate the ED environment and enhance the patient experience—from registration to treatment and administration.
As medical technology becomes more portable, it is more readily available bedside to support interventions that must be completed as quickly as possible to optimize outcomes.
“The outcomes of many time-sensitive health conditions, such as heart attacks, trauma, and stroke, are highly dependent on the speed of treatment,” says Mik Pietrzak, MD, Director of Strategy and Technology at MedStar Institute for Innovation in Washington, D.C. “As technology continues to become more miniaturized and portable, we may be able to eliminate some spaces because everything will essentially be bedside and movable from room to room.”
For example, the i-STAT handheld blood testing system developed by Abbott Point of Care delivers laboratory-quality test results in a fraction of the space required by a traditional ED lab.
Technology also facilitates a more pleasant patient experience through integration of high-definition TVs, WiFi-enabled tablets, and videoconferencing capabilities to comfort and distract patients (and family members) while waiting to receive emergency care.
5. Greater outreach to the community.
Long considered the hospital’s front door, emergency departments are being threatened by competition from retail pharmacies and big-box stores that are offering various levels of medical services, such as the ability to consult a pharmacist, nurse, or nurse practitioner.
“Before the changes in healthcare brought on by the Affordable Care Act, a facility didn’t have to worry too much about the welcoming nature of its emergency department,” says Skanska’s Quirk. “Now, the whole business of healthcare is becoming more consumer-based and market-focused.”
To survive in this increasingly perilous healthcare jungle, hospital systems are actively reestablishing the ED’s role as an accessible, welcoming community resource.
 The three-story, 75,000-sf Marion Emergency Care Center at Texas Health Harris Methodist Hospital, in Fort Worth, nearly tripled the space of the facility it replaced and increased patient capacity from 56 beds to 100. The $57.7 million facility, designed by HKS, opened in January 2014. Photo: Daryl Shields / HKS
The three-story, 75,000-sf Marion Emergency Care Center at Texas Health Harris Methodist Hospital, in Fort Worth, nearly tripled the space of the facility it replaced and increased patient capacity from 56 beds to 100. The $57.7 million facility, designed by HKS, opened in January 2014. Photo: Daryl Shields / HKS
Hospitals are aggressively marketing their emergency services as convenient alternatives to new “retail” healthcare providers, which can’t offer the resources of a full-service ED. Healthcare systems are countering with consumer-focused marketing, branding, and signage campaigns.
Hospitals are also working hard to reduce waiting times in their EDs—one of the greatest sources of patient dissatisfaction.
SSM Health Care, a health network serving the St. Louis region, offers an online ED registration system for reserving a specific time at any of its seven hospitals. The option is intended for the 40% of ED visits that involve non-life-threatening conditions.
Introduced about three years ago, the self-scheduling system currently registers about 10% of SSM’s annual ED visits. The system lets the ED staff know ahead of time what’s wrong with the patient and when he or she will arrive so that they can allocate staff and room resources accordingly.
“If someone uses the system once, they tend to use it again and tell family members and others about it,” says Wayne Laramie, RN, Regional Coordinator of Emergency Services for SSM Health Care. “It sells itself.”
6. Enhanced preparation for catastrophic events.
When it comes to responding to catastrophic natural disasters, accidents with multiple casualties, acts of terrorism, and infectious disease outbreaks, emergency departments are on the front lines.
These events often require additional capacity to accommodate a sudden massive influx of patients; in the case of a biological or infectious disease event, they also demand resources and protocols for segregating affected patients from the general hospital population.
“Now that we’re in the age of heightened awareness of infectious diseases, all hospitals are going to reawaken to the need to demonstrate to patients and staff that they have the ability to control infections—and that it starts right at the front door,” says HKS’s Lennon.
He and colleague David Vincent have advanced a model of an “all-risk-ready” ED, which provides for:
- Separate portals or chambers at the entrance to screen—and possibly decontaminate—individuals before they access the facility.
- Installation of advanced air-delivery systems similar to those used in clean rooms at manufacturing facilities to precisely control the flow of air from outside and within the facility.
- Use of surface-applied, self-decontaminating agents in treatment rooms.
- Placement of a colored strip along treatment room walls that would encompass high-touch items, such as light switches, electrical and medical gas outlets, and paper towel dispensers, so that they can be efficiently sanitized.
“The key is not to lose capacity during event-based conditions, when you actually need to increase capacity,” says Vincent.
7. The rise of the freestanding emergency center.
Emergency care is reaching beyond the confines of hospitals and into the communities where existing and future patient populations reside.
More than 400 freestanding emergency centers now dot the U.S. healthcare landscape. Frequently affiliated with hospital systems, these standalone facilities offer the medical resources of a traditional ED. They are often collocated in medical office buildings that house ancillary services such as physician offices, walk-in imaging capabilities, and ambulatory surgery centers.
Freestanding EDs should not be confused with urgent care centers. As state-licensed facilities, freestanding EDs must fulfill the same architectural and equipment requirements of full-service EDs. They must operate 24/7, have on-site emergency physicians, and provide round-the-clock lab and imaging capabilities.
 The new ED at Parkland Hospital, Dallas, features 140-sf universal, acuity-adaptable, same-handed treatment rooms. HDR and Corgan designed the rooms to adapt to rapidly changing patient needs and to help providers deliver care faster and more efficiently. Photo courtesy HDR
The new ED at Parkland Hospital, Dallas, features 140-sf universal, acuity-adaptable, same-handed treatment rooms. HDR and Corgan designed the rooms to adapt to rapidly changing patient needs and to help providers deliver care faster and more efficiently. Photo courtesy HDR
For hospital systems, these centers offer an opportunity to expand their footprint, deliver care to underserved populations, and reduce crowding in their hospital-based EDs without incurring the capital costs of building a new acute-care hospital.
Mercy Health, a Cincinnati-based healthcare system serving Ohio and Kentucky, has expanded its market reach by constructing several freestanding EDs in outlying suburban and rural areas.
Mercy’s proprietary market research revealed that the two most important factors in the choice of an emergency facility were proximity and waiting time, says Meszaros.
Mercy also asked people if they might be concerned if an ED facility was not physically attached to a hospital. Not a problem, says Meszaros: “We found that folks were comfortable if the ED is affiliated with a hospital that has a positive reputation.”
Contractors are applying special techniques to control costs in the construction of freestanding EDs. “We try to prefabricate as much of the building as we can offsite in a factory and deliver it to the site completed,” says Skanska’s Quirk. Prefab, he says, is pushing quality up, bringing costs down, and shortening schedules “so that hospitals can improve speed to market and start delivering care to people faster.”
At Rookwood Medical Center, a freestanding ED in suburban Cincinnati, the project team prefabricated all of the overhead MEP racks at an offsite location. “This allowed construction workers to assemble, insulate, dry wall, and test the racks in a climate-controlled environment while working in late winter and early spring,” says Quirk. “This approach not only created a safer atmosphere for construction workers by minimizing work done overhead and on ladders, but it also cut down on material waste.”
Freestanding EDs are also emerging in urban areas. When New York City’s St. Vincent’s Hospital closed in 2010, it left a healthcare void for the residents of Manhattan’s West Village neighborhood.
North Shore–LIJ Health System stepped in and renovated the former Maritime Union Hall into the Lenox Hill HealthPlex, a medical facility that includes Manhattan’s first freestanding ED.
Opening in 2014, the ED treated more than 10,000 patients in its first five months of operation and exceeded the 90th percentile in patient satisfaction surveys conducted by Press Ganey, a third-party healthcare research firm.
The facility includes private treatment rooms with telemedicine capabilities and recliner chairs with iPads for patients awaiting test results. “We can call in specialists from anywhere in our health system to come right into the room with us on a secure monitor,” says Alex Hellinger, Executive Director of Lenox Hill HealthPlex. “Patients have their own interactive monitor where they can watch TV, go on the Web, or use Skype so a family member can be part of their care.”
Sound-absorbing ceiling panels and hands-free communications badges contribute to an uncharacteristically calm environment. Hellinger says that even when the ED is fully occupied, it doesn’t look busy to patients. “It’s not the chaotic scene that you see in most EDs,” he says.
ED facilities like the Lenox Hill HealthPlex reflect a new age of healthcare that puts the emphasis on convenience, speed, and keeping people healthy, says Jeff Brand, AIA, EDAC, National Healthcare Practice Area Leader at Perkins Eastman, which designed the facility.
“What once would have been a medical office building is now a high-technology, robust, mixed-use building, tethered to a main hospital system by ambulances,” he says. “These facilities are successful because they’re fine-tuned to provide just what a particular community needs.”
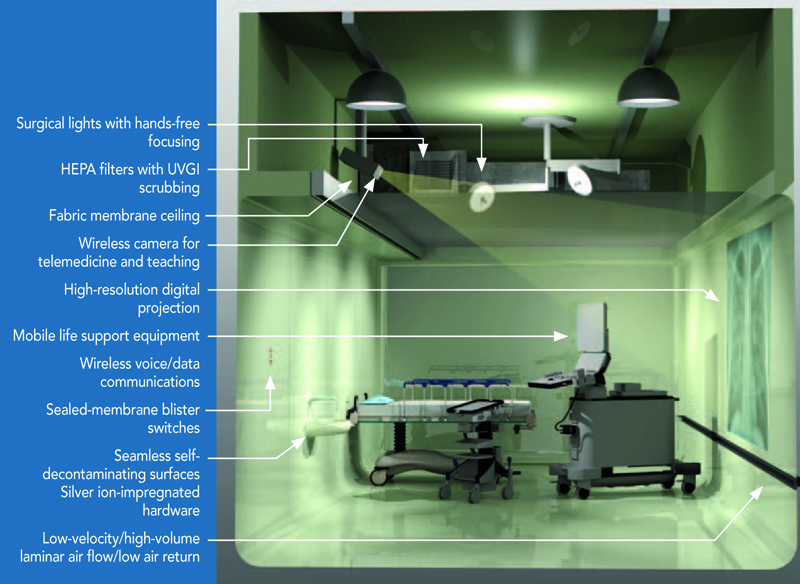 An immune room concept developed by ED design specialists at HKS includes a seamless, self-decontaminating environment where everything is portable. Special ventilation systems protect patients and hospital employees from potential exposure to airborne diseases. In today’s environment, hospital EDs must demonstrate that they can control infections, says HKS’s Jim Lennon. Illustration courtesy HKS
An immune room concept developed by ED design specialists at HKS includes a seamless, self-decontaminating environment where everything is portable. Special ventilation systems protect patients and hospital employees from potential exposure to airborne diseases. In today’s environment, hospital EDs must demonstrate that they can control infections, says HKS’s Jim Lennon. Illustration courtesy HKS
The editors would like to thank the following experts for their assistance with this report:
Jeff Brand, AIA, EDAC
National Healthcare Practice Area Leader
Perkins Eastman
New York, N.Y.
Alex Hellinger
Executive Director
Lenox Hill HealthPlex
New York, N.Y.
Jim Lennon, AIA, ACHA, LEED AP
Associate Principal
HKS, Inc.
San Diego, Calif.
Patti Meszaros
Director of Facility Planning
Mercy Health
Cincinnati, Ohio
Kurt Nyberg
Project Director
McCarthy Building Companies
Phoenix, Ariz.
Mik Pietrzak, MD
Director of Strategy and Technology
MedStar Institute for Innovation
Washington, D. C.
Andrew Quirk
National Director, Healthcare Center of Excellence
Skanska USA Building
Nashville, Tenn.
Marvina Williams, RN
Healthcare Clinical Operations Expert
Perkins+Will
Atlanta, Ga.
Related Stories
Healthcare Facilities | May 24, 2019
Beyond the corner store: Where retail health is headed
New players are redefining what retail health might look like by embracing technologies including mobile apps, telehealth, and artificial intelligence.
Healthcare Facilities | May 16, 2019
ASU Health Futures Center combines a novel design and approach to learning
The trapezoidal shape of the building is an eco-friendly feature.
Healthcare Facilities | May 9, 2019
Construction of new children’s hospital addition in NW Florida had to weather several storms
Patient and staff care were primary concerns during this 25-month project, says its GC.
Healthcare Facilities | May 3, 2019
The healthcare sector is turning to drones to supplement medical services
Leo A Daly’s Miami studio envisions a drone-powered hospital that enhances resilience to natural disasters.
| Apr 26, 2019
Greenwich Hospital upgrades boilers to improve operational efficiency
Greenwich Hospital, in Greenwich, Conn., chooses new Miura boilers.
Healthcare Facilities | Apr 15, 2019
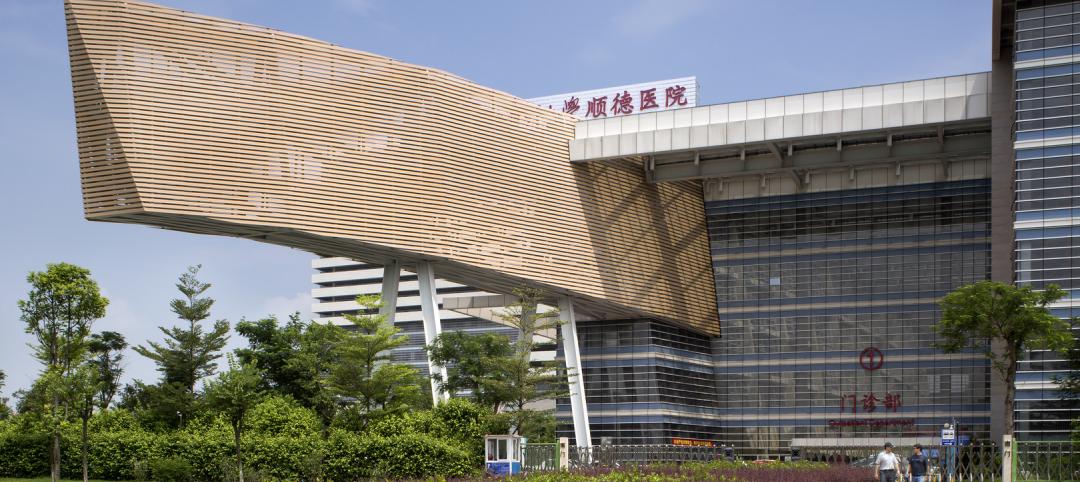
It’s official: China opens first green hospital, designed by HMC Architects
Shunde Hospital of Southern Medical University is the official pilot green hospital for development of China’s green guide for hospital design.
Healthcare Facilities | Apr 12, 2019
New health pavilion completes on the Health Education Campus at Case Western Reserve University
Foster + Partners designed the facility.
Healthcare Facilities | Apr 9, 2019
How healthcare organizations can leverage design and culture's symbiotic relationship
The relationship between workplace design and company culture isn’t all that different from a tango.
Healthcare Facilities | Apr 3, 2019
Patients will actively seek out lower-cost and virtual healthcare in the future
Mortenson’s latest study finds that Millennials’ inclinations toward technological solutions are changing how care is and will be delivered.
Healthcare Facilities | Apr 3, 2019
Children’s Hospital at Sacred Heart addition includes 175,000 sf of new construction
HKS Architects designed the addition.