Healthcare consumers are just as likely to factor in convenience as they do cost when deciding where to seek care and from whom, according to a new survey of 4,037 American adults about their attitudes and preferences as patients.
The survey, conducted from April 19-28 by JLL, in many ways confirms the obvious: that older generations seek preventive care more often than younger generations; that insurance coverage is a primary driver for choosing a provider or hospital; and that the quality of service affects the patient experience.
Nearly eight of 10 of the survey’s respondents had received at least one type of non-dental care in the last year. Women, who accounted for 51% of the survey’s respondents, are more likely to receive care overall, but men are more likely to receive emergency care.
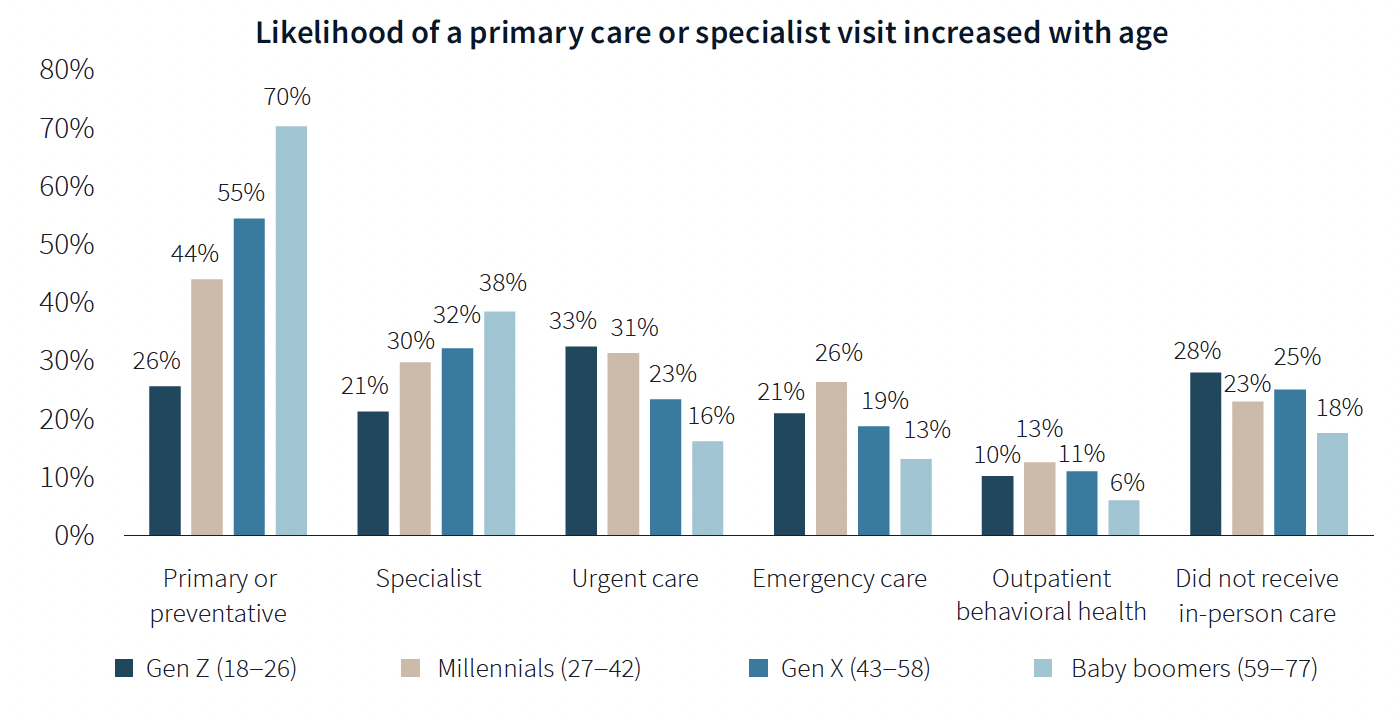
The likelihood of a primary care or specialist visit increases with age: 80% of adults 65 years or older have two or more chronic conditions that require continuous care. More than 70% of Baby Boomers (who accounted for 29% of the survey’s respondents) had received primary or preventive care within the last year, compared to only 26% of Generation Z.
Younger generations are more reactive than preventive in their healthcare decisions, borne out by the survey’s finding that Millennials and Gen Zs (43% of the survey's respondents) are more likely to receive urgent care, emergency care, and outpatient behavioral healthcare than older adults.
Proximity to patients counts
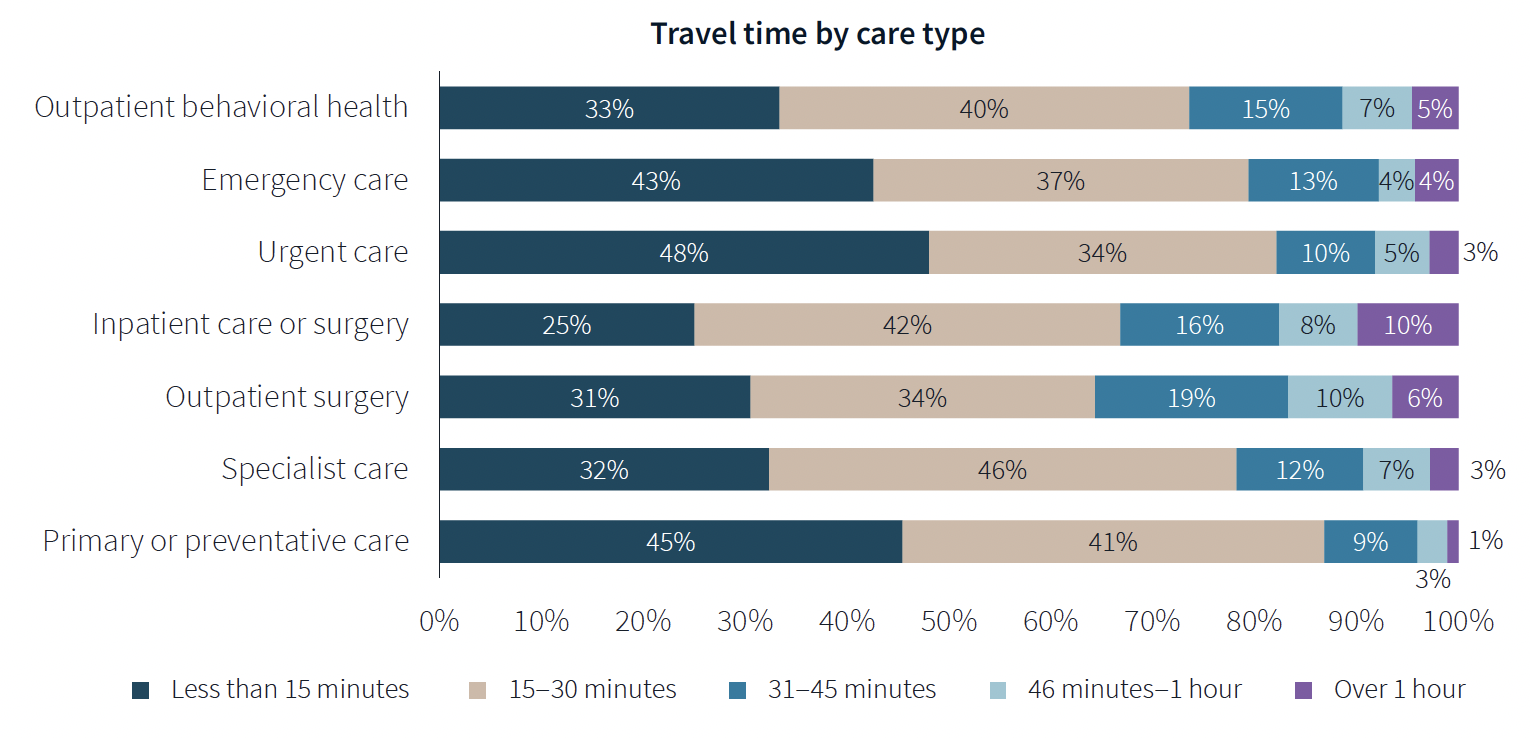
When care is urgently needed, “decision factors are simplified,” the survey states, and location and proximity of care are ranked higher as decision-making factors. But even outside of emergencies, convenience ranks high among factors for patients seeking care.
There’s no denying that cost is always in the background of any healthcare decision. “Accept my insurance” was the most common factor for choosing a provider among the survey’s respondents. (82% of participants has private insurance, and 81% has public insurance.)
Two-fifths of respondents said they travel less than 15 minutes to receive care, and nearly eight of 10 respondents travel less than 30 minutes. Among those with appointments in standalone medical offices, 85% ranked location as convenience, which the survey suggested indicates the advantages of a dispersed location strategy.
“A strong location strategy can improve reach for health systems and physician practices and potentially improve care outcomes,” JLL writes. “But there is a balance between convenience and cost—health systems need to balance the benefits of being close to their target population with the cost of a new facility or doctors’ time in transit from a local clinic to the hospital.”
Convenience is also key both in location and in being able to navigate to care. Patients want to get to care quickly and get on with their day. Ease of parking and ability to navigate the facility also affected a facility’s net positive score in the survey.
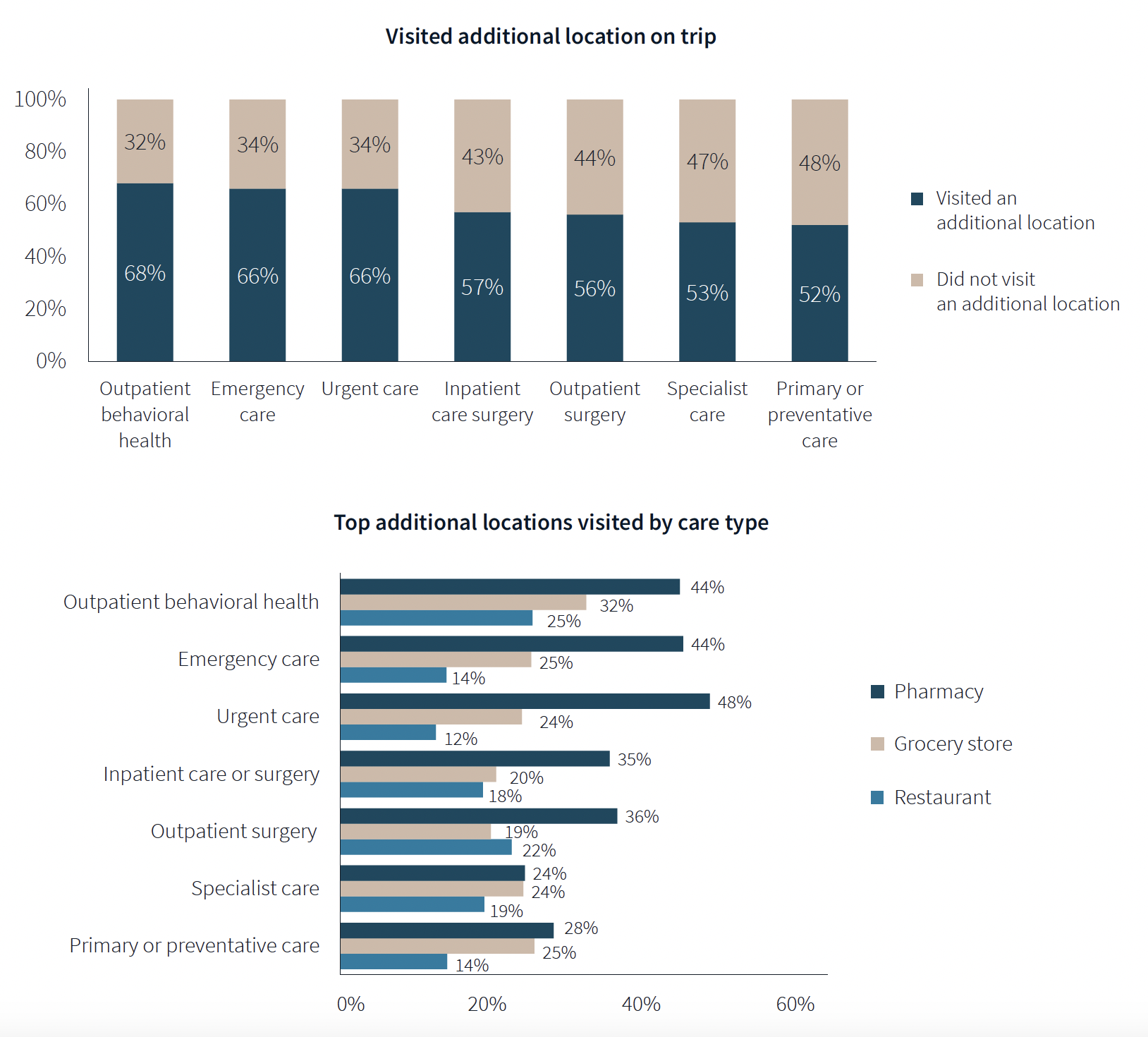
One of the survey’s more revealing findings is that nearly three-fifths of respondents—58%—went to another location—such as a pharmacy, or an urgent clinic—as part of their trip for healthcare.
Word of mouth often defines quality of care
Patients seem to be open to diverse care choices. For example, 29% said they have visited a retail clinic, such as a CVS, and would do so again. Gen Z and Millennials are more likely to frequent retail clinics for their convenient appointment schedules and shorter wait times.
More than two-fifths of respondents—42%—had a telehealth appointment within the last year, which was slightly down from the 45% in JLL’s 2022 survey. This year’s poll also found that 29% of telehealth appointments led to an in-person visit.
More than 40% of respondents ranked “reputation of quality” among the top five factors for choosing care. But where they get their impressions about quality varies.
Referrals play a larger role in specialist, outpatient surgery and inpatient care. Recommendations from friends ranked most highly for behavioral health, given the personal nature of such care, and was ranked in the top five by 31% of respondents. Younger patients, who “have yet to develop brand loyalty,” according to the survey, are more likely to rely on word-of-mouth recommendations than older patients for whom hospital systems’ reps matter more.
Outpatient surgery and primary care ranked highest for provider satisfaction; emergency care ranked lowest. Participants ranked their experiences on 12 aspects of care, and the biggest gap between “promoters” and “detractors” was for the service level of providers. Primary care had the highest net provider score, with 86% of respondents ranking its care as “attentive.”
Some amenities draw patients
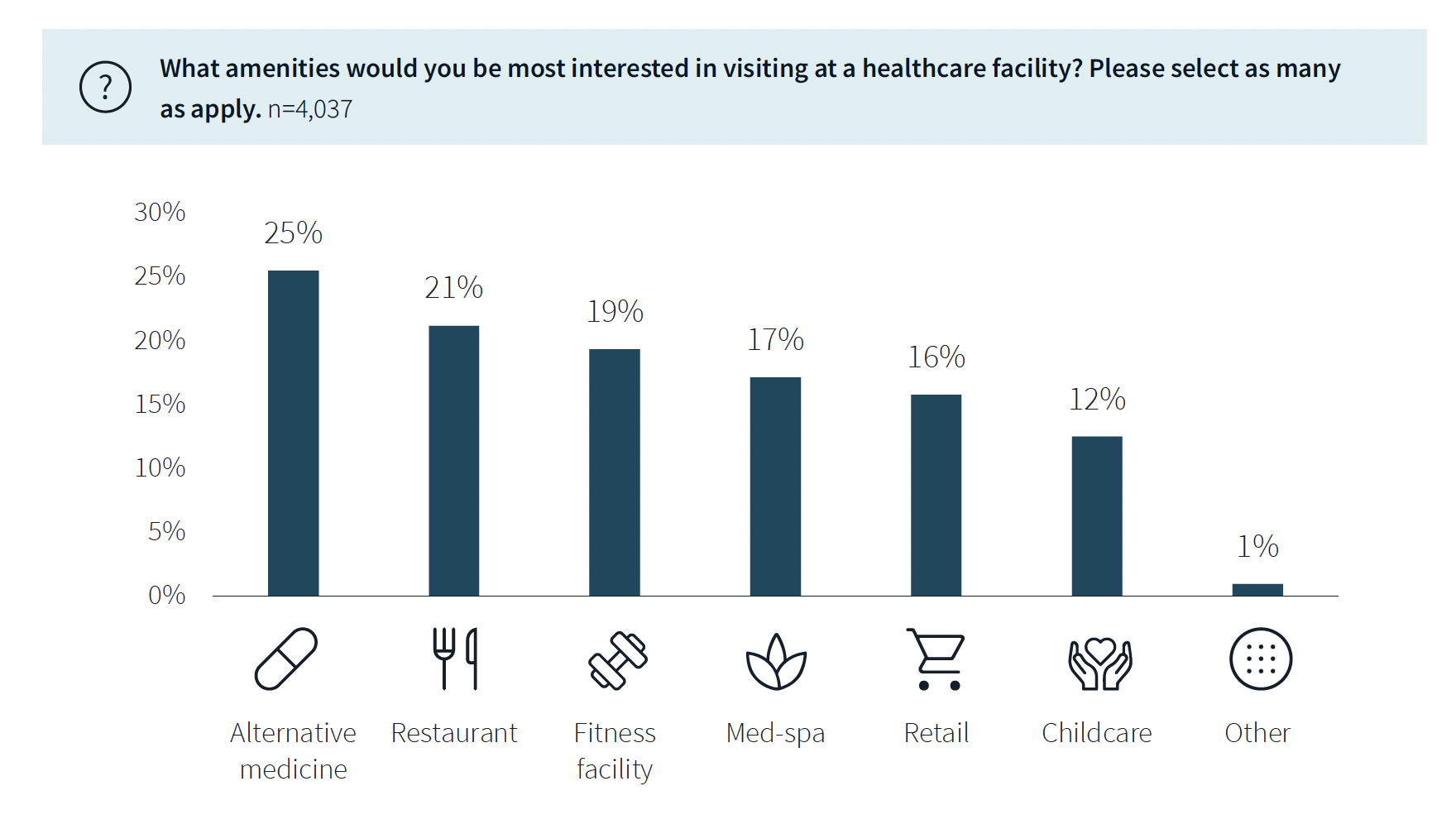
While not a decision-making factor, amenities do attract some patients. Among the survey’s respondents, 63% said they would be interested in visiting a healthcare facility with an additional amenity, such as alternative medicine, a restaurant, fitness center, or spa. (This inclination was more evident among younger respondents.)
The overall quality of facilities, including the comfort of their waiting rooms, can impact a patient’s choice, especially for inpatient, urgent, and emergency care. The survey also found that urban locations have lower favorability rankings for their facilities, signaling room for improvement. (Just under half—48%—of respondents live in the suburbs.)
Related Stories
| Dec 29, 2014
New mobile unit takes the worry out of equipment sterilization during healthcare construction [BD+C's 2014 Great Solutions Report]
Infection control, a constant worry for hospital administrators and clinical staffs, is heightened when the hospital is undergoing a major construction project. Mobile Sterilization Solutions, a mobile sterile-processing department, is designed to simplify the task. The technology was named a 2014 Great Solution by the editors of Building Design+Construction.
| Dec 29, 2014
HealthSpot station merges personalized healthcare with videoconferencing [BD+C's 2014 Great Solutions Report]
The HealthSpot station is an 8x5-foot, ADA-compliant mobile kiosk that lets patients access a network of board-certified physicians through interactive videoconferencing and medical devices. It was named a 2014 Great Solution by the editors of Building Design+Construction.
BIM and Information Technology | Dec 28, 2014
The Big Data revolution: How data-driven design is transforming project planning
There are literally hundreds of applications for deep analytics in planning and design projects, not to mention the many benefits for construction teams, building owners, and facility managers. We profile some early successful applications.
| Dec 28, 2014
AIA course: Enhancing interior comfort while improving overall building efficacy
Providing more comfortable conditions to building occupants has become a top priority in today’s interior designs. This course is worth 1.0 AIA LU/HSW.
| Dec 2, 2014
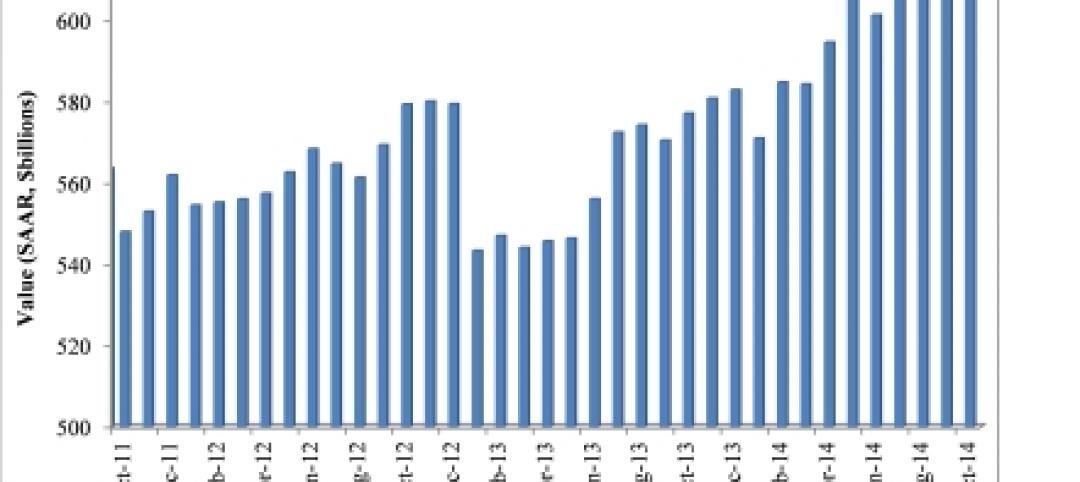
Nonresidential construction spending rebounds in October
This month's increase in nonresidential construction spending is far more consistent with the anecdotal information floating around the industry, says ABC's Chief Economist Anirban Basu.
| Dec 1, 2014
How public-private partnerships can help with public building projects
Minimizing lifecycle costs and transferring risk to the private sector are among the benefits to applying the P3 project delivery model on public building projects, according to experts from Skanska USA.
| Nov 25, 2014
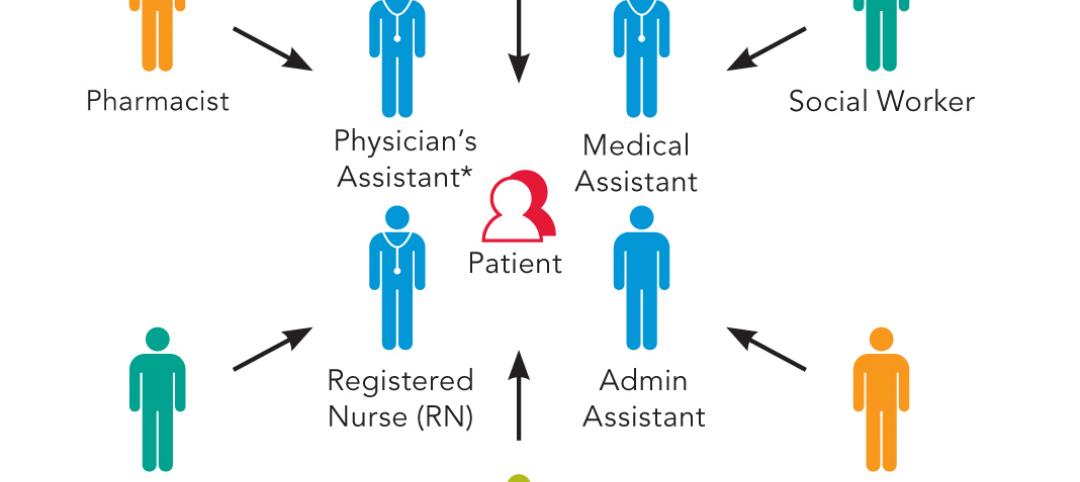
Emerging design and operation strategies for the ambulatory team in transition
As healthcare systems shift their care models to be more responsive to patient-centered care, ambulatory care teams need to be positioned to operate efficiently in their everyday work environments, write CannonDesign Health Practice leaders Tonia Burnette and Mike Pukszta.
| Nov 20, 2014
Lean Led Design: How Building Teams can cut costs, reduce waste in healthcare construction projects
Healthcare organizations are under extreme pressure to reduce costs, writes CBRE Healthcare's Lora Schwartz. Tools like Lean Led Design are helping them cope.
| Nov 18, 2014
5 big trends changing the world of academic medicine
Things are changing in healthcare. Within academic medicine alone, there is a global shortage of healthcare professionals, a changing policy landscape within the U..S., and new view and techniques in both pedagogy and practice, writes Perkins+Will’s Pat Bosch.
| Nov 14, 2014
Haskell acquires FreemanWhite, strengthens healthcare design-build business
The combination expands Haskell’s geographic presence by adding FreemanWhite’s offices in Chicago, Charlotte, Nashville, and San Diego. FreemanWhite will retain its name and brand.