Healthcare consumers are just as likely to factor in convenience as they do cost when deciding where to seek care and from whom, according to a new survey of 4,037 American adults about their attitudes and preferences as patients.
The survey, conducted from April 19-28 by JLL, in many ways confirms the obvious: that older generations seek preventive care more often than younger generations; that insurance coverage is a primary driver for choosing a provider or hospital; and that the quality of service affects the patient experience.
Nearly eight of 10 of the survey’s respondents had received at least one type of non-dental care in the last year. Women, who accounted for 51% of the survey’s respondents, are more likely to receive care overall, but men are more likely to receive emergency care.
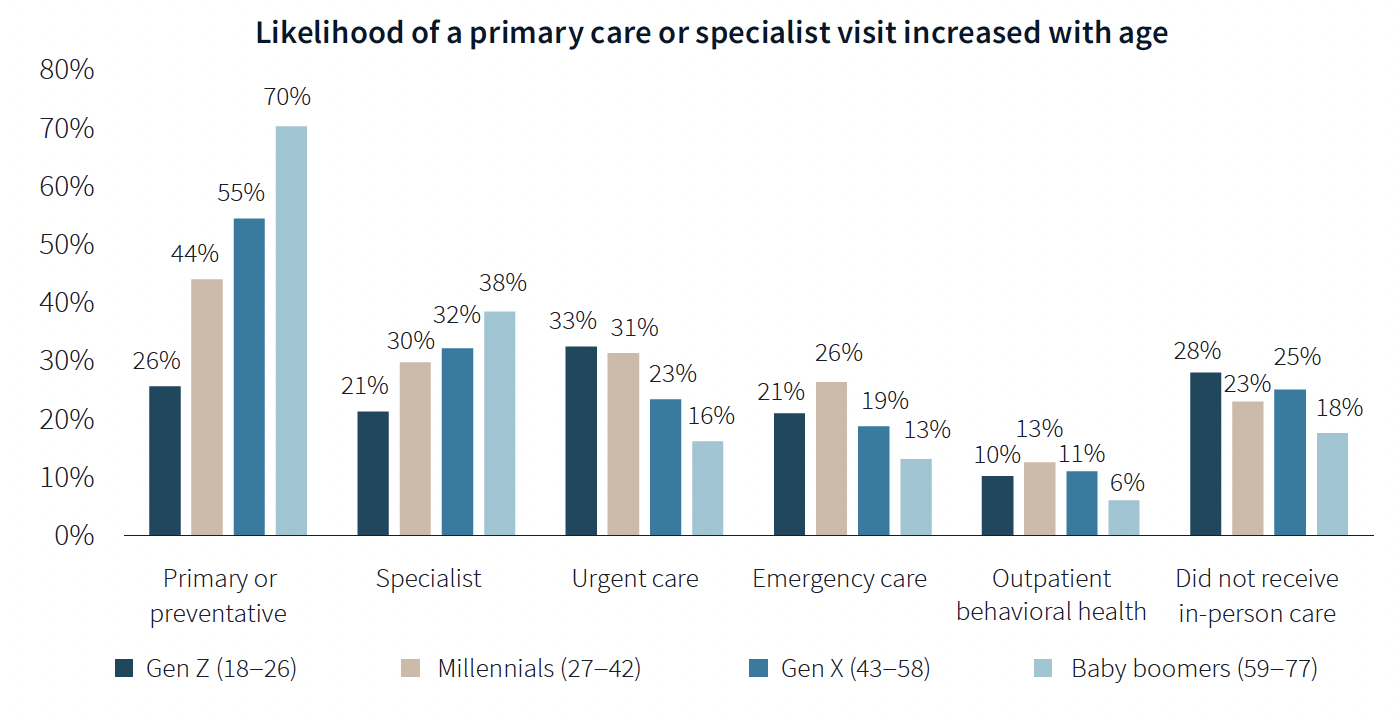
The likelihood of a primary care or specialist visit increases with age: 80% of adults 65 years or older have two or more chronic conditions that require continuous care. More than 70% of Baby Boomers (who accounted for 29% of the survey’s respondents) had received primary or preventive care within the last year, compared to only 26% of Generation Z.
Younger generations are more reactive than preventive in their healthcare decisions, borne out by the survey’s finding that Millennials and Gen Zs (43% of the survey's respondents) are more likely to receive urgent care, emergency care, and outpatient behavioral healthcare than older adults.
Proximity to patients counts
When care is urgently needed, “decision factors are simplified,” the survey states, and location and proximity of care are ranked higher as decision-making factors. But even outside of emergencies, convenience ranks high among factors for patients seeking care.
There’s no denying that cost is always in the background of any healthcare decision. “Accept my insurance” was the most common factor for choosing a provider among the survey’s respondents. (82% of participants has private insurance, and 81% has public insurance.)
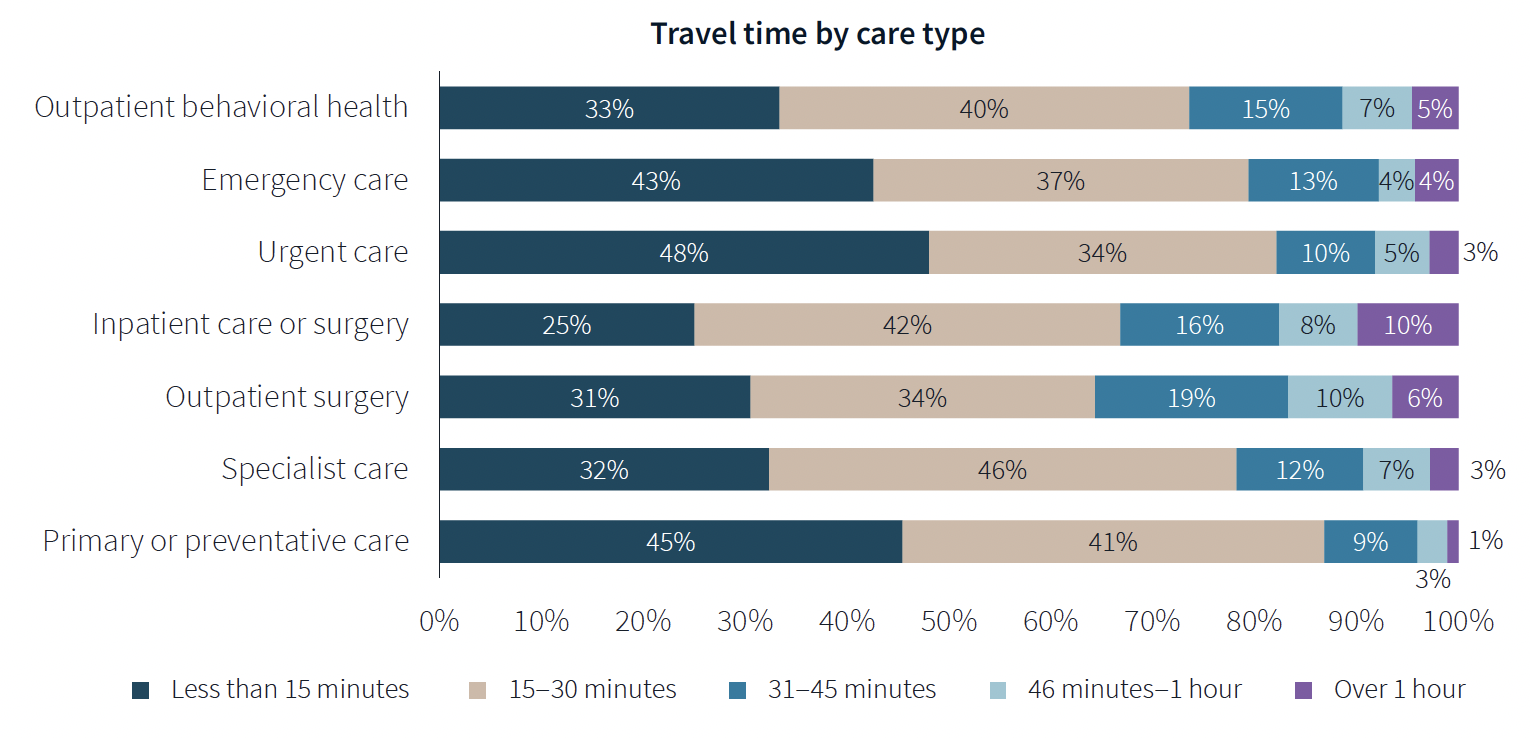
Two-fifths of respondents said they travel less than 15 minutes to receive care, and nearly eight of 10 respondents travel less than 30 minutes. Among those with appointments in standalone medical offices, 85% ranked location as convenience, which the survey suggested indicates the advantages of a dispersed location strategy.
“A strong location strategy can improve reach for health systems and physician practices and potentially improve care outcomes,” JLL writes. “But there is a balance between convenience and cost—health systems need to balance the benefits of being close to their target population with the cost of a new facility or doctors’ time in transit from a local clinic to the hospital.”
Convenience is also key both in location and in being able to navigate to care. Patients want to get to care quickly and get on with their day. Ease of parking and ability to navigate the facility also affected a facility’s net positive score in the survey.
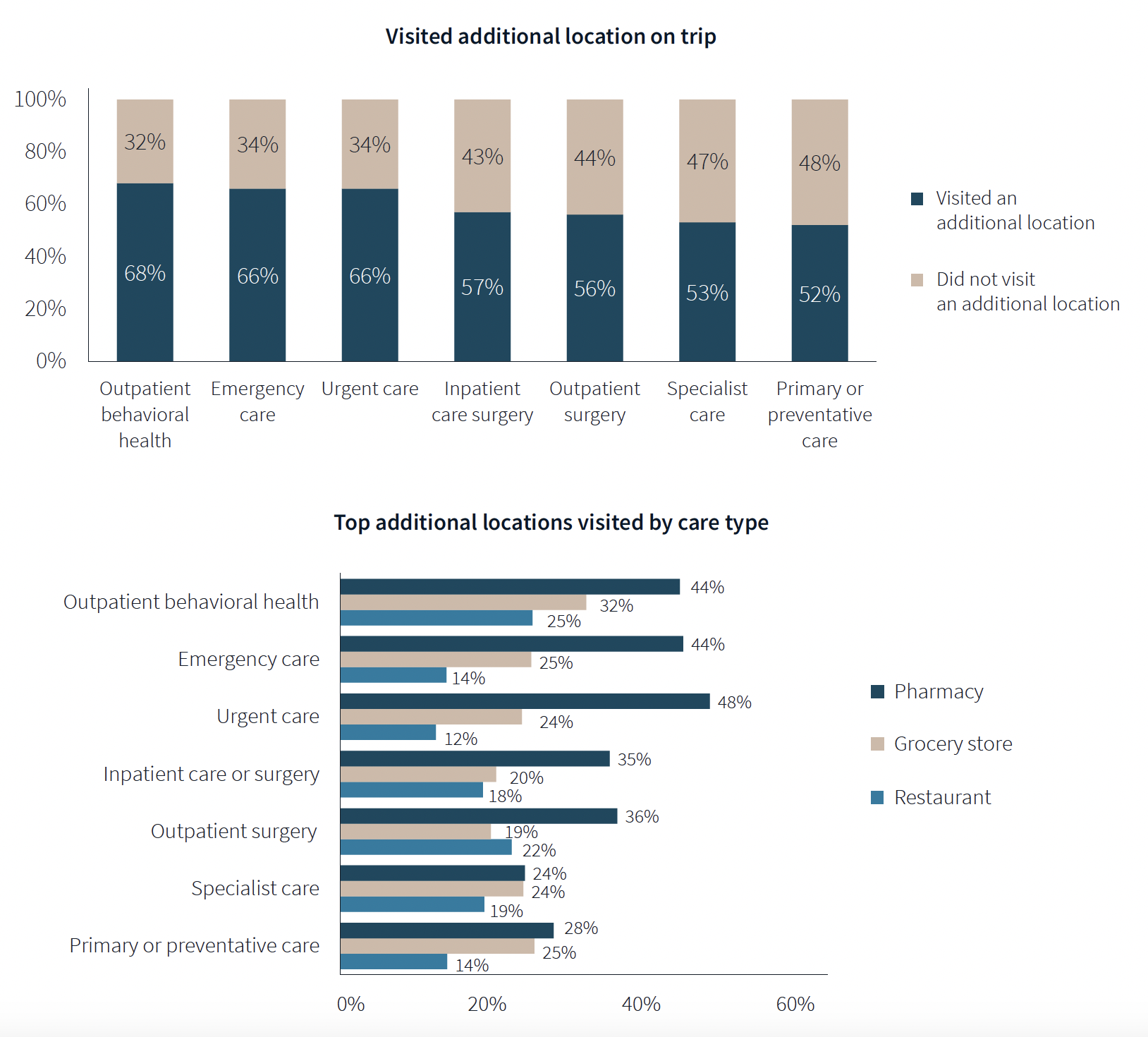
One of the survey’s more revealing findings is that nearly three-fifths of respondents—58%—went to another location—such as a pharmacy, or an urgent clinic—as part of their trip for healthcare.
Word of mouth often defines quality of care
Patients seem to be open to diverse care choices. For example, 29% said they have visited a retail clinic, such as a CVS, and would do so again. Gen Z and Millennials are more likely to frequent retail clinics for their convenient appointment schedules and shorter wait times.
More than two-fifths of respondents—42%—had a telehealth appointment within the last year, which was slightly down from the 45% in JLL’s 2022 survey. This year’s poll also found that 29% of telehealth appointments led to an in-person visit.
More than 40% of respondents ranked “reputation of quality” among the top five factors for choosing care. But where they get their impressions about quality varies.
Referrals play a larger role in specialist, outpatient surgery and inpatient care. Recommendations from friends ranked most highly for behavioral health, given the personal nature of such care, and was ranked in the top five by 31% of respondents. Younger patients, who “have yet to develop brand loyalty,” according to the survey, are more likely to rely on word-of-mouth recommendations than older patients for whom hospital systems’ reps matter more.
Outpatient surgery and primary care ranked highest for provider satisfaction; emergency care ranked lowest. Participants ranked their experiences on 12 aspects of care, and the biggest gap between “promoters” and “detractors” was for the service level of providers. Primary care had the highest net provider score, with 86% of respondents ranking its care as “attentive.”
Some amenities draw patients
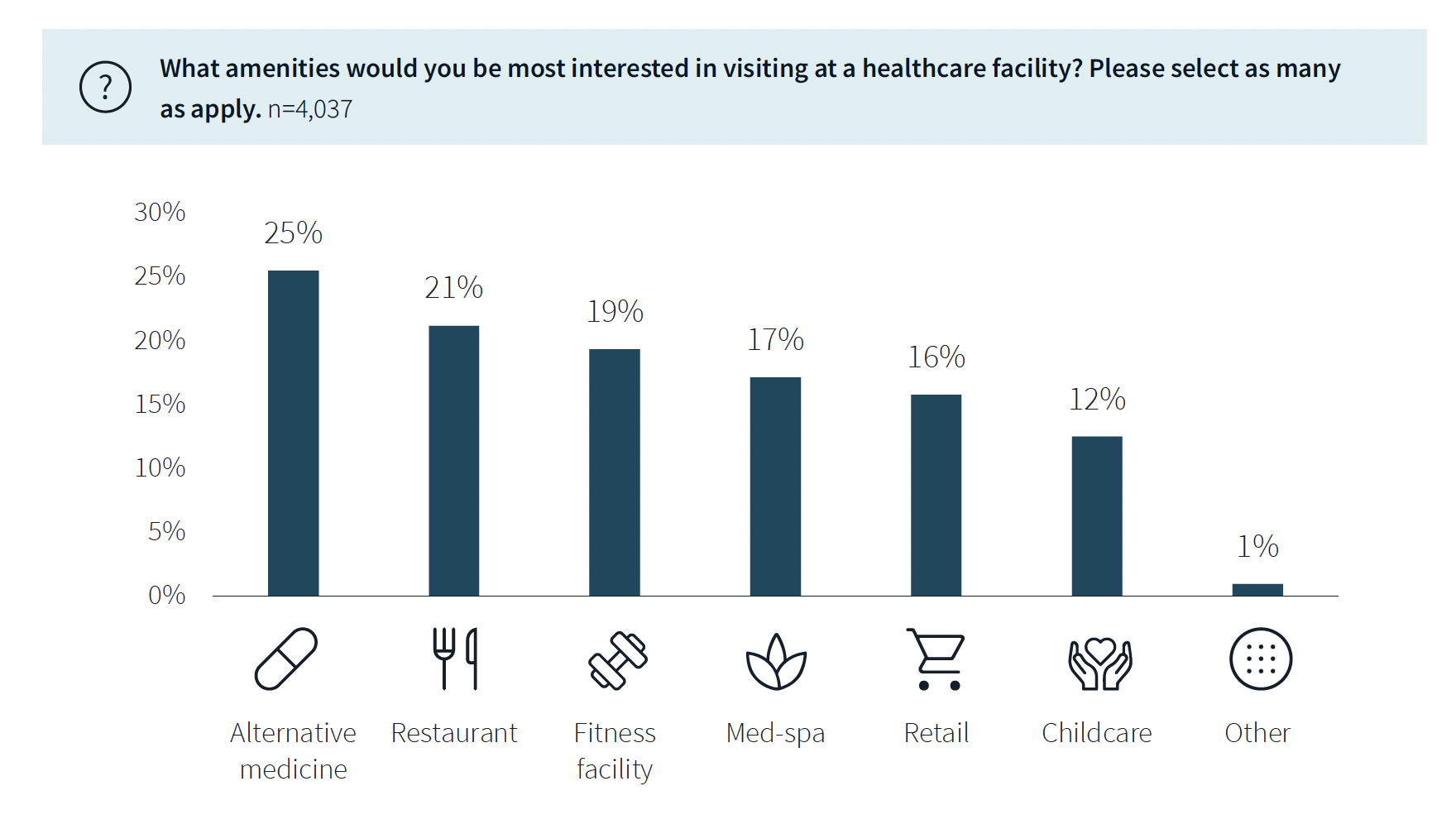
While not a decision-making factor, amenities do attract some patients. Among the survey’s respondents, 63% said they would be interested in visiting a healthcare facility with an additional amenity, such as alternative medicine, a restaurant, fitness center, or spa. (This inclination was more evident among younger respondents.)
The overall quality of facilities, including the comfort of their waiting rooms, can impact a patient’s choice, especially for inpatient, urgent, and emergency care. The survey also found that urban locations have lower favorability rankings for their facilities, signaling room for improvement. (Just under half—48%—of respondents live in the suburbs.)
Related Stories
| May 1, 2013
Groups urge Congress: Keep energy conservation requirements for government buildings
More than 350 companies urge rejection of special interest efforts to gut key parts of Energy Independence and Security Act
| May 1, 2013
World’s tallest children’s hospital pushes BIM to the extreme
The Building Team for the 23-story Lurie Children’s Hospital in Chicago implements an integrated BIM/VDC workflow to execute a complex vertical program.
| Apr 30, 2013
Tips for designing with fire rated glass - AIA/CES course
Kate Steel of Steel Consulting Services offers tips and advice for choosing the correct code-compliant glazing product for every fire-rated application. This BD+C University class is worth 1.0 AIA LU/HSW.
| Apr 30, 2013
Healthcare lighting innovation: Overhead fixture uses UV to kill airborne pathogens
Designed specifically for hospitals, nursing homes, child care centers, and other healthcare facilities where infection control is a concern, the Arcalux Health Risk Management System (HRMS) is an energy-efficient lighting fixture that doubles as a germ-killing machine.
| Apr 24, 2013
North Carolina bill would ban green rating systems that put state lumber industry at disadvantage
North Carolina lawmakers have introduced state legislation that would restrict the use of national green building rating programs, including LEED, on public projects.
| Apr 24, 2013
Los Angeles may add cool roofs to its building code
Los Angeles Mayor Antonio Villaraigosa wants cool roofs added to the city’s building code. He is also asking the Department of Water and Power (LADWP) to create incentives that make it financially attractive for homeowners to install cool roofs.
| Apr 10, 2013
ASHRAE publishes second edition to HVAC manual for healthcare facilities
The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) has published a second edition of its “HVAC Design Manual for Hospitals and Clinics.”
| Apr 2, 2013
6 lobby design tips
If you do hotels, schools, student unions, office buildings, performing arts centers, transportation facilities, or any structure with a lobby, here are six principles from healthcare lobby design that make for happier users—and more satisfied owners.
| Apr 2, 2013
4 hospital lobbies provide a healthy perspective
A carefully considered entry zone can put patients at ease while sending a powerful branding message for your healthcare client. Our experts show how to do it through four project case studies.