A recent poll of healthcare providers found that 85% agree that most patients will not require an in-person physician evaluation by 2021. Virtual doctor visits will be common, smartphones and wearable sensors will be used widely to record a patient’s health information, and patients will have greater access to self-serving their health needs via technology equipped unmanned kiosks.
These are some of the predictions from the Mortenson Leadership Series Healthcare Study, the construction firm’s fourth in the last six years. The study is based on a poll of more than 900 healthcare professionals, facilities leaders, and architects who support them, conducted during last year’s ASHE Planning, Design, and Construction Summit.
While most of the study’s findings weren’t surprising, they confirm trends about Millennials’ healthcare expectations, how and where healthcare institutions will be investing, the role of technology in healthcare, and what roadblocks might lie ahead for project management.

Millennials' preferences for how they receive healthcare are having a major impact on how health systems are investing. Image: Mortenson
One thing is certain: patients are taking more ownership of their health. Eighty-three percent of the healthcare providers polled observe that patients are far more willing these days to shop for lower-cost care options. By 2021, 85% predict that providers will screen patients first to guide them to the appropriate treatment. And that won’t necessarily be toward a medical office or clinic.
One of the biggest disparities between the 2018 and 2015 surveys was the responses to the question about how common virtual doctors would be in three years’ time. Last year, 88% responded to this question affirmatively, compared to 63% in 2015. And 85% in the 2018 surveyed participants thought that most patients don’t require an in-person physician evaluation, versus 49% in 2015.
As one 2018 respondent noted, “Millennials expect immediate access. This access will drive how we design facilities as well as garner a new age of telehealth.” Two-fifths of healthcare providers and architects mentioned that virtual telemedicine and self-service treatments would be typical delivery care within the next decade, with much less reliance on physical structures to deliver goods and services.
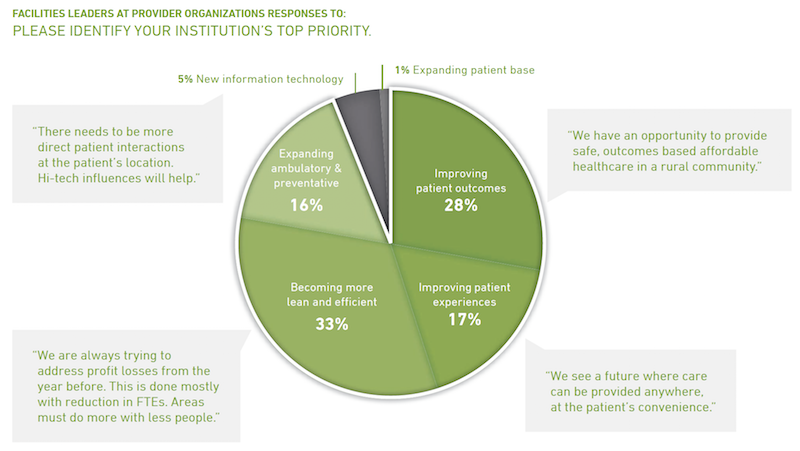
Healthcare facilities managers say their institutions must become leaner to grapple with insufficient project resources. Many see opportunities in reducing waste and energy consumption. Image: Mortenson
More than two-fifths (44%) of architects polled also said that Millennials’ expectations about the need for more integration and utilization of technology is impacting healthcare and its facilities, followed by 22% who cited the demand for convenience and virtual care. “Less acute, more ambulatory. Less invasive procedures. More virtual … diagnosis and treatments,” stated one respondent.
Two thirds of facilities leaders polled said that their institutions would invest more over the next two to three years. But 35% added that their biggest challenge continues to be insufficient money and resources (including receiving adequate payments for services rendered), followed by “growing pains” (18%) and project delivery (17%).
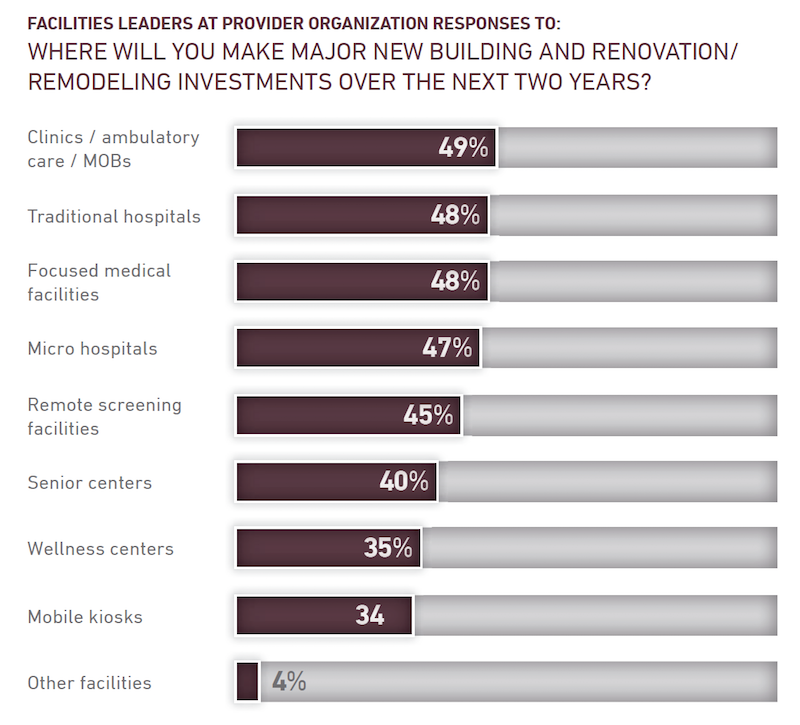
Nearly half of facilities leaders polled say their healthcare systems continue to invest in clinics, ambulatory care centers, and medical offices. Image: Mortenson
Nearly all of the facilities leaders see significant opportunities to eliminate waste and reduce energy use.
Despite all of speculation about virtual care expressed in the study, 49% of facilities leaders said their institutions would be making major investments in clinics, ambulatory care, and MOBs, followed by traditional hospitals and focused medical facilities (48% each), microhospitals (47%), and remote screening facilities (45%).
The respondents were evenly split about how much their institutions might spend over the next two years, with 33% each projecting moderate, substantial, or flat growth.
The study includes a section about the Affordable Care Act. Fewer respondents in 2018 than in 2015 thought the legislation had done enough to address the country’s long-term healthcare needs. And between 94% and 97% of those polled last year said that the Act still needed “significant changes or revisions,” had created uncertainty for their institutions, and had challenged their organization’s near-term financial condition.
Related Stories
| May 5, 2011
Hospitals launch quiet campaigns to drown out noise of modern medicine
Worldwide, sound levels inside hospitals average 72 decibels during the day and 60 decibels at night, which far exceeds the standard of 40 decibels or less, set by the World Health Organization. The culprit: modern medicine. In response, hospitals throughout Illinois and the U.S. are launching "quiet campaigns" that include eliminating intercom paging, replacing metal trash cans, installing sound-absorbing flooring and paneling, and dimming lights at night to remind staff to keep their voices down.
| Apr 14, 2011
USGBC debuts LEED for Healthcare
The U.S. Green Building Council (USGBC) introduces its latest green building rating system, LEED for Healthcare. The rating system guides the design and construction of both new buildings and major renovations of existing buildings, and can be applied to inpatient, outpatient and licensed long-term care facilities, medical offices, assisted living facilities and medical education and research centers.
| Apr 13, 2011
Virginia hospital’s prescription for green construction: LEED Gold
Rockingham Memorial Hospital in Harrisonburg, Va., is the commonwealth’s first inpatient healthcare facility to earn LEED Gold. The 630,000-sf facility was designed by Earl Swensson Associates, with commissioning consultant SSRCx, both of Nashville.
| Apr 12, 2011
Mental hospital in Boston redeveloped as healthcare complex
An abandoned state mental health facility in Boston’s prestigious Longwood Medical Area is being transformed into the Mass Mental Health Center, a four-building mixed-use complex that includes a mental health day hospital, a clinical and office building, a medical research facility for Brigham and Women’s Hospital, and a residential facility.
| Mar 17, 2011
Perkins Eastman launches The Green House prototype design package
Design and architecture firm Perkins Eastman is pleased to join The Green House project and NCB Capital Impact in announcing the launch of The Green House Prototype Design Package. The Prototype will help providers develop small home senior living communities with greater efficiency and cost savings—all to the standards of care developed by The Green House project.
| Mar 14, 2011
Renowned sustainable architect Charles D. Knight to lead Cannon Design’s Phoenix office
Cannon Design is pleased to announce that Charles D. Knight, AIA, CID, LEED AP, has joined the firm as principal. Knight will serve as the leader of the Phoenix office with a focus on advancing the firm’s healthcare practice. Knight brings over 25 years of experience and is an internationally recognized architect who has won numerous awards for his unique contributions to the sustainable and humanistic design of healthcare facilities.
| Mar 11, 2011
Renovation energizes retirement community in Massachusetts
The 12-year-old Edgewood Retirement Community in Andover, Mass., underwent a major 40,000-sf expansion and renovation that added 60 patient care beds in the long-term care unit, a new 17,000-sf, 40-bed cognitive impairment unit, and an 80-seat informal dining bistro.
| Mar 11, 2011
Research facility added to Texas Medical Center
Situated on the Texas Medical Center’s North Campus in Houston, the new Methodist Hospital Research Institute is a 12-story, 440,000-sf facility dedicated to translational research. Designed by New York City-based Kohn Pedersen Fox, with healthcare, science, and technology firm WHR Architects, Houston, the building has open, flexible labs, offices, and amenities for use by 90 principal investigators and 800 post-doc trainees and staff.
| Mar 11, 2011
Mixed-income retirement community in Maryland based on holistic care
The Green House Residences at Stadium Place in Waverly, Md., is a five-story, 40,600-sf, mixed-income retirement community based on a holistic continuum of care concept developed by Dr. Bill Thomas. Each of the four residential floors houses a self-contained home for 12 residents that includes 12 bedrooms/baths organized around a common living/social area called the “hearth,” which includes a kitchen, living room with fireplace, and dining area.