The Program of All-Inclusive Care for the Elderly (PACE) is gaining momentum across the country as a cost-effective and compassionate way to support the desires of frail elders to live in their homes and communities and avoid premature nursing home placement. With 118 PACE centers in 32 states, the program is considered the gold standard of care for seniors.
A One Stop Shop
The PACE center is the heart of the program and serves as a "one stop shop" for enrollees, otherwise known as Participants, to receive care and services tailored to meet individual needs. Participants visit the PACE center as needed, up to five days per week, where they receive a majority of care and services. Additionally, transportation is provided to and from the PACE center daily or services can be provided at home to support participant independence. Care is coordinated, provided and paid for by the PACE Interdisciplinary Team (IDT) that knows each Participant’s needs and desires and tailors care and services accordingly. A typical PACE center is comprised of a fully functioning and equipped primary care clinic, adult day center and rehabilitation therapy gym. In addition, it includes find dining areas, large group activity spaces, a PT and rehab space, meditation spaces and a medical clinic capable of primary care. Participants can watch TV, play organized games, relax in one of the many quiet spaces or simply talk to one another. The IDT of nurses, social workers, dieticians, physical therapists, occupational therapists, transportation and primary care physicians is available to attend to a Participant’s needs.
Design and Planning Considerations
Averaging 18,000SF – 22,000SF, the ideal PACE facility is a single story building with a large outdoor covered portico allowing for safe all-weather loading and unloading of Participants. Corridors are approximately 8 foot wide to accommodate the above average number of wheelchairs, as well as other mobility devices, and have a minimal number of corridor bends. Participant socialization spaces are adjacent to one another to reduce walking distances and are connected via large openings rather than doors. While dependent on the population demographics, specific areas are also designed for Participants with dementia related behaviors. Each center has a kitchen for meal preparation and/or serving. Many existing centers buy ready-made meals from vendors and simply reheat in the kitchen thus saving time in preparation and potentially saving significant costs in not having to design and construct a full commercial kitchen.

The fully functioning clinic provides basic primary care to Participants only. Family members are not able to use the clinic as an Urgent Care center or equivalent. The clinic space has an average of 4-6 exam rooms that are enlarged to accommodate wheel chairs. Modular casework is preferred over custom millwork to help budget constraints as modular can offer 40% savings. Medical equipment requirements are not as intensive as an acute care hospital, again supporting the smaller modular casework concept.
For Participant activity areas, a large oven and microwave are included to allow for baking demonstrations or competitions. Several computer terminals with internet access are also available. A patio or landscaped area provides Participants the opportunity to be outdoors to relax or participate in a variety of outdoor activities.
As expected in all healthcare facilities, the safetyand security of Participants is critical. A PACE center’s safety features include an electronic access control system to prohibit wandering and elopement. Additionally, all participant spaces are equipped with a nurse call system that can alert staff in the case of an emergency. Nurse call stations are located in bathrooms, bathing and personal care areas, exam rooms and activity spaces.
In addition to Participant program spaces, each center includes meeting spaces for the IDT. In order for the 11 member IDT to plan, provide and coordinate direct care for Participants, the center must include an adequate large space for daily group meetings as well as multiple smaller work spaces. Staff and administrative work areas are typically located away from Participant program spaces. As opposed to constructing private offices, many staff work spaces are shared work stations that save space and reduce cost.
Business Fundamentals
Ideally, the PACE program will relieve hospital emergency departments of minor medical issues not warranting an ED visit and will reduce hospitalization rates by improving access to care. National research also shows Participants having reduced morbidity and mortality rates and a higher quality of life compared to those living in nursing homes. PACE also provides flexibility to families by relieving the burden of care without taking a family member away from their home. In addition to the high family satisfaction ratings, the program has very low disenrollment. Despite the recognition of the model’s success, PACE programs have grown incrementally and care for only a fraction of their potential population mainly due to CMS regulations.
Conclusion
The benefits of PACE are very apparent and the program is gaining momentum across the country. There is hope that new regulation will provide even more operational flexibility to support expansion and allow PACE programs to operate more competitively in the post-health care reform marketplace. Identifying opportunities to relieve ED volume, reduce cost, improve access and most importantly increase quality of life for our aging population is critical to solving our healthcare dilemma. PACE has proven to be a successful component and vital part of this equation.
Related Stories
| May 1, 2014
Super BIM: 7 award-winning BIM/VDC-driven projects
Thom Mayne's Perot Museum of Nature and Science and Anaheim's new intermodal center are among the 2014 AIA TAP BIM Award winners.
| Apr 29, 2014
USGBC launches real-time green building data dashboard
The online data visualization resource highlights green building data for each state and Washington, D.C.
| Apr 16, 2014
Upgrading windows: repair, refurbish, or retrofit [AIA course]
Building Teams must focus on a number of key decisions in order to arrive at the optimal solution: repair the windows in place, remove and refurbish them, or opt for full replacement.
| Apr 9, 2014
How patient-centered medical homes can help healthcare providers and patients
Beyond reducing the number of uninsured Americans, the Affordable Care Act is driving new types of healthcare facilities, especially patient-centered medical homes.
| Apr 9, 2014
Steel decks: 11 tips for their proper use | BD+C
Building Teams have been using steel decks with proven success for 75 years. Building Design+Construction consulted with technical experts from the Steel Deck Institute and the deck manufacturing industry for their advice on how best to use steel decking.
| Apr 2, 2014
The new model of healthcare facility management
A growing number of healthcare organizations are moving to an integrated real estate model in an effort to better manage costs, respond to regulatory requirements, and support changes in patient care delivery.
| Apr 2, 2014
8 tips for avoiding thermal bridges in window applications
Aligning thermal breaks and applying air barriers are among the top design and installation tricks recommended by building enclosure experts.
| Mar 26, 2014
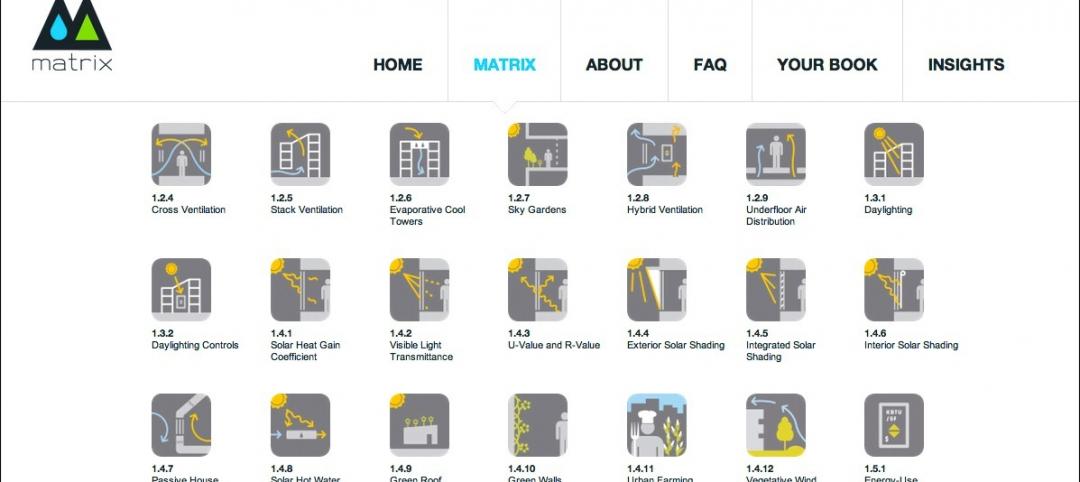
Callison launches sustainable design tool with 84 proven strategies
Hybrid ventilation, nighttime cooling, and fuel cell technology are among the dozens of sustainable design techniques profiled by Callison on its new website, Matrix.Callison.com.
Sponsored | | Mar 25, 2014
Johns Hopkins chooses SLENDERWALL for a critical medical facility reconstruction
After decades of wear, the hand-laid brick envelope of the Johns Hopkins nine-story Nelson/Harvey inpatient facility began failing. SLENDERWALL met the requirements for renovation.
| Mar 20, 2014
Common EIFS failures, and how to prevent them
Poor workmanship, impact damage, building movement, and incompatible or unsound substrate are among the major culprits of EIFS problems.