At some point in our lives, many of us will have to make a difficult decision regarding the long-term care of a spouse or parent. Someone may even have to make this decision for us one day. When a family member can no longer be cared for in their current home, they require specialized care that is only available in a long-term care center. These facilities are outfitted with the care providers, the skilled personnel, the equipment, and the appropriately “designed” environment suited to the frail elderly.
Developers usually build long-term care facilities in the suburbs where land is less expensive. These centers tend to be distant from the existing communities where new residents may have lived for many years. There are good reasons we have developed these facilities. Many older people need 24-hour supervised care because they are on multiple medications, and they may have some form of dementia along with comorbidities including congestive heart failure, COPD, pulmonary disease, diabetes, and a high risk of injury from falls. In short, they need specialized care. These facilities also need to achieve the economies of scale needed to make limited funding and staff numbers work. Therefore, they tend to be large facilities, often with several hundred beds.
But for many residents, these centers are alien to the way they have lived their lives. I believe many residents feel like they have been yanked out of the places they call home and stuck somewhere else miles away. Their long-term facility isolates them from the extended family and those who can support them, cutting them off from the communities where they found comfort. The scale of the facility makes the residents more dependent on the institution for services and food, limiting choice for when and what one can eat or how often one can bathe.
Today, we are locked in the let’s-get-everyone-in-one-place model, and the result is these large institutional centers.
But what if it didn’t have to be this way?
Is this the most effective way to do this? And is this best for the person who needs the care? Can we move away from large centers for the frail elderly in the suburbs? Could we find a way of providing those services on a more distributed basis within the community? For example, could we create a model where people stay in their own home or stay in their own neighborhood?
From a community development perspective, how would this model—call it Distributed Care—impact plan development and impact land use bylaws and transportation?
Technology to the rescue
What’s driving the possibility of Distributed Care? Technology. Connected care—making use of internet-connected devices and miniaturized equipment—has reached a point of sophistication and affordability that enables us to provide care remotely. Even now, we can monitor and predict (by utilizing Artificial Intelligence) someone at risk of falling at home. Predictive software can recognize behavior that will result in a fall if it continues over time and deliver a warning or give a remote caregiver a chance to intervene.
In Distributed Care, we will plan houses and smaller residences so they are connected to an internet of care—wireless smart devices that allow monitoring wellness and help in predicting when residents may be at risk. This would mean recognizing signs of dietary risk such as rapid weight loss, or recognizing a gait change that indicates a risk of falling, or changes in speech that signal other troubles. Other services can be provided by delivery or scheduled visits to the residence.
Of course, society is not going to stop building long-term care centers. There will continue to be a role for them in managing complex cases, for those in long-term care with psychiatric issues, and extremely complicated health issues.
Barriers
Truthfully, there are barriers to this Distributed Care model. There are land-use bylaws that may prevent the use of a former single family home as a small commercial care facility, for example. There may be code restrictions to meet in addition to these zoning considerations. But these laws can be changed or planned around.
Distribution of services
Most promising, I believe, are the ways in which alternative distributed models will impact the delivery of healthcare services. Right now, if the family caregiver notices their elderly mother isn’t feeling well they are most likely headed to the nearest hospital emergency room. But statistically, it’s likely that her issue is simple, perhaps a case of dehydration or an adjustment in meds. So, why is that simple case tying up the emergency department, which is intended to care for the acutely ill? We are beginning to design for more integrated approaches, which better account the needs of the elderly. One example: a long-term care facility with an accessible primary care unit embedded in it to take care of day-to-day issues and access to a nearby hospital emergency room for more immediate and serious cases. Senior living co-location with acute care environments integrating long-term and primary care in a distributed model has much to offer.
Today, if someone shows up at a community care clinic with a possible heart issue, they’re sent off to an emergency room to see the cardiologist there. Technology makes it possible for health care professionals to conduct virtual visits, inter-hospital consultations, and even remote diagnoses. Wouldn’t it be better if the cardiologist could come to the clinic through remote presence technology and perform the consult? The cardiologist simply logs in from a computer and observes the patient, who is wired up and monitored as normal, but now transmitting data to the remote specialist. This type of care enables more flexibility for providing acute care within the distributed care model.
This technology may sound complex and it is, but it’s relatively inexpensive—most of the elements for remote presence examinations are available now. The challenge is changing our mindset about where the point of care is and what model of long-term care is best for those who require it. We’ll need a multi-disciplinary approach as designers, planners, and healthcare experts to adapt to this model.
Four examples of Distributed Senior Care
- The Greenhouse Model for senior care (as seen here) aims to reinvent the way long-term care is delivered by creating smaller home-like environments where seniors have private rooms and baths, have the ability to move freely, are given the opportunity to develop meaningful relationships with other residents and staff, and can even assist in preparing their own meals.
- Seniors can continue living with a degree of independency and comfort in a home-like, private room. With changes in land-use regulations, they may be able to reside in homes converted to commercial care. (The opening rendering of a resident room at the St. John Specialty Care Centre offers an example.)
- The “Laneway House,” or “Granny Pod,” are small independent living arrangements. These secondary suites can be built for seniors in the backyards of family homes or built and rented by unrelated property owners. Home care support teams can provide service based on individual needs.
- Deliberately-planned “age-friendly” communities support the entire spectrum of life, from birth to death. Developing senior living within mixed-use developments provides seniors access to lively community spaces, amenities, and public transit, helping to reduce the isolation felt with traditional/ institutional suburban long-term care homes.
 International Hotel Senior Housing and St. Mary’s Catholic School Complex in San Francisco, California. It is an example of deliberately-planned “age-friendly” communities. (Stantec Architecture with Greg Roja & Associates, Herman & Coliver Architecture, and Tai Associates).
International Hotel Senior Housing and St. Mary’s Catholic School Complex in San Francisco, California. It is an example of deliberately-planned “age-friendly” communities. (Stantec Architecture with Greg Roja & Associates, Herman & Coliver Architecture, and Tai Associates).More from Author
Stantec | Jul 18, 2024
Why decarbonizing hospitals smartly is better than electrification for healthcare design
Driven by new laws, regulations, tariffs, ESG goals, and thought leaders in the industry itself, healthcare institutions are embracing decarbonization to meet 2050 goals for emissions reductions.
Stantec | Jun 18, 2024
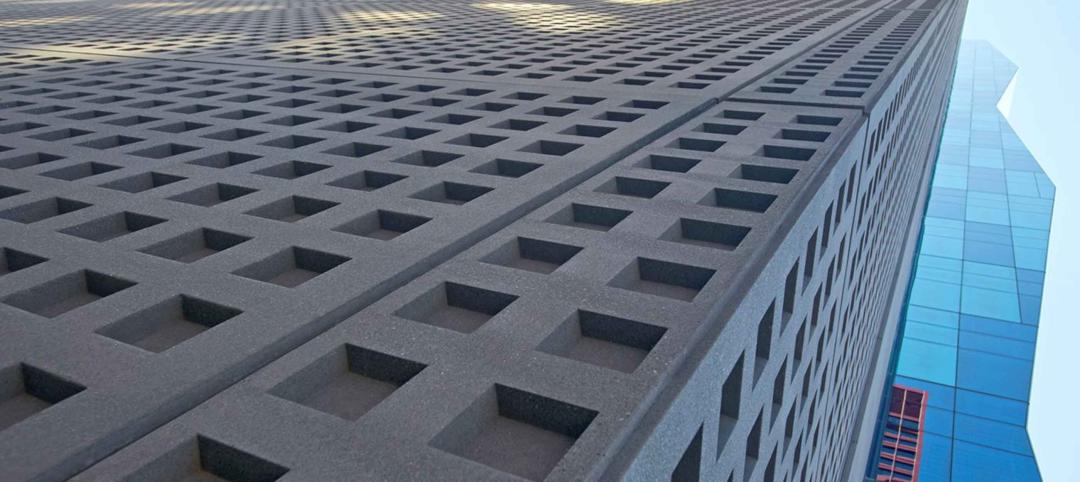
Could ‘smart’ building facades heat and cool buildings?
A promising research project looks at the possibilities for thermoelectric systems to thermally condition buildings, writes Mahsa Farid Mohajer, Sustainable Building Analyst with Stantec.
Stantec | Jun 8, 2024
8 ways to cool a factory
Whichever way you look at it—from a workplace wellness point of view or from a competing for talent angle—there are good reasons to explore options for climate control in the factory workplace.
Stantec | Apr 18, 2024
The next destination: Passive design airports
Today, we can design airports that are climate resilient, durable, long-lasting, and healthy for occupants—we can design airports using Passive House standards.
Stantec | Mar 18, 2024
A modular construction solution to the mental healthcare crisis
Maria Ionescu, Senior Medical Planner, Stantec, shares a tested solution for the overburdened emergency department: Modular hub-and-spoke design.
Stantec | Nov 20, 2023
8 strategies for multifamily passive house design projects
Stantec's Brett Lambert, Principal of Architecture and Passive House Certified Consultant, uses the Northland Newton Development project to guide designers with eight tips for designing multifamily passive house projects.
Stantec | Apr 10, 2023
Implementing human-centric design in operations and maintenance facilities
Stantec's Ryan Odell suggests using the human experience to advance OMSF design that puts a focus on wellness and efficiency.
Stantec | Jul 6, 2022
5 approaches to a net zero strategy that communities can start right now
Whether your community has started on a plan or is still considering net zero, now is the time for all of us to start seriously addressing climate change.
Stantec | Feb 14, 2022
5 steps to remake suburbs into green communities where people want to live, work, and play
Stantec's John Bachmann offers proven tactic for retrofitting communities for success in the post-COVID era.
Stantec | Feb 8, 2022
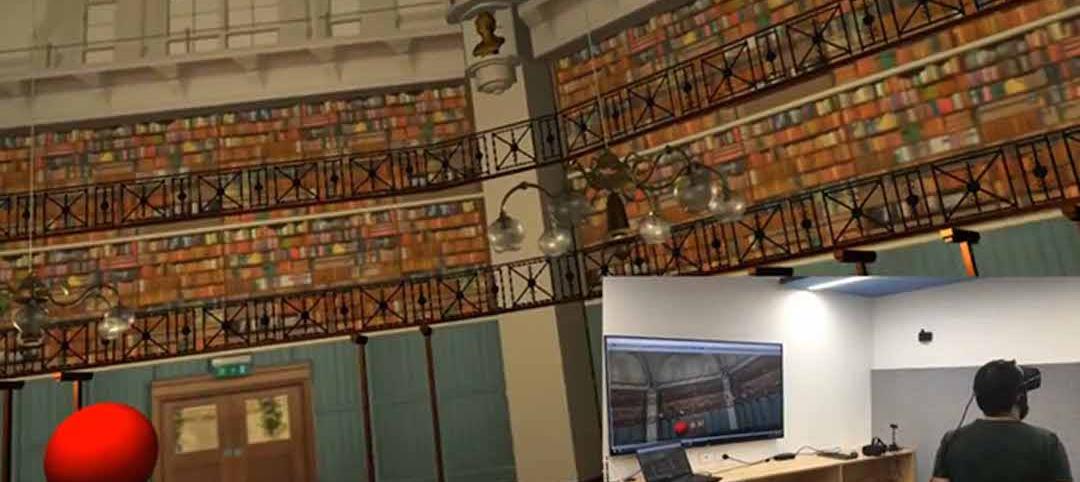
How gaming technology is changing the way we design for acoustics
Adding 3D sound from gaming engines to VR allows designers to represent accurate acoustic conditions to clients during design.