Several states and municipalities are aggressively investigating the conversion of hotels into makeshift hospitals in order to free up much-needed beds in hospitals for patients who have contracted COVID-19.
Leo A Daly is currently negotiating with several hoteliers about converting large portfolios of hotels into healthcare facilities that follow the firm’s Hotel2Hospital prototype, which would conform with design guidelines released last week to state governments by the U.S. Army Corps of Engineers, which relax some of the hospital safety standards.
The Nebraska-based firm is working with several national design-build contractors to get such conversions started.
“Hospitals and hotels have several common characteristics that make this a promising solution,” says Joshua Theodore, ACHE, EDAC, vice president and global health practice leader for Leo A Daly. “Both are comprised of private, individual rooms with a dedicated toilet and HVAC systems. Air handling is critical to patient and staff safety in infectious disease environments, so hotel rooms have an instant advantage over other typologies in terms of viability.”
Leo A Daly did not disclose the healthcare systems or contractors it is speaking or working with about its conversion proposals.
Three modes for hotel-to-hospital conversions for COVID-19
The average hotel could accommodate up to 80 patients, Leo A Daly estimates. And many are located near existing hospitals.
Hotels also have food service, cleaning service, waste removal and laundry service, all of which are critical to any inpatient healthcare facility, says Theodore. He notes, too, that hotels are currently experiencing high vacancy rates that are likely to persist until the coronavirus dissipates.
Hotel2Hospital offers three adaptive reuse models. Each will require different levels of biocontainment and intervention to the physical building.
Reuse Model 1 would be to quarantine suspected or asymptomatic COVID-19 patients. Reuse Model 2 would be for symptomatic isolation of patients with underlying risk factors who are already sick but aren’t likely to require full ICU inpatient treatment. (Ventilators and telemetry would likely be used for this facility type). Reuse Model 3 would be for non-infected patients who currently are being hospitalized and could potentially receive treatment in alternative care environments so as to free up hospital beds for more acute COVID-19 patients.
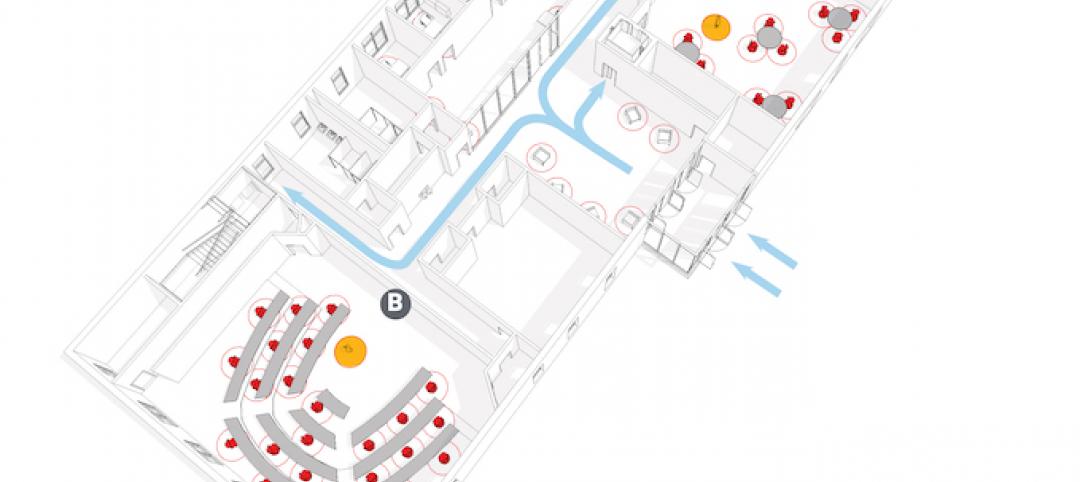
For Reuse Model 1, the hotel furniture could be used, but the bed would require medical linens. A nurse station would be created in a room opposite the elevator core, and the floor would also have an eye/hand washing station. In this model, the reception and office areas in the lobby would be repurposed for patient check-in. Any retail area would be converted to a pharmacy. And offices could be converted to lab space. The converted room would also need to be modified with a larger exhaust fan system to its existing toilet exhaust duct system to create negative pressure.
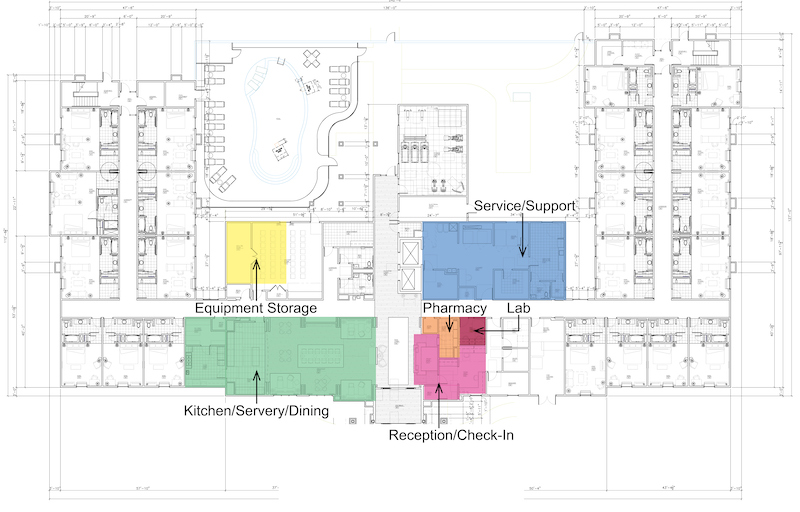
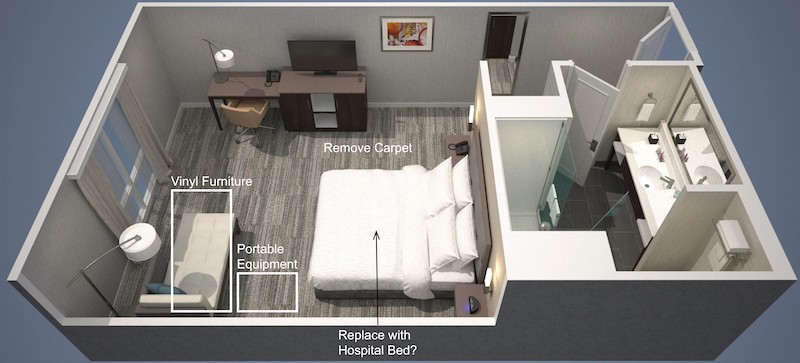
The Reuse Model 2 would, among other changes, convert the hotel's reception area into a patient check-in, and make retail and office spaces into pharmacies and labs. The carpeting in the rooms and corridors would be removed.
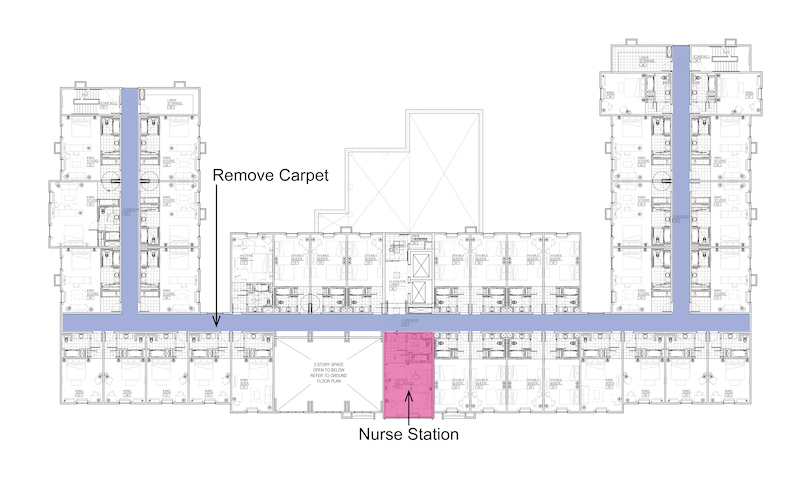
A conversion of a hotel to Reuse Model 2 would undertake the measures spelled out for Reuse Model 1, and then some. Carpeting, polishes, and concrete floor sealing would be removed from the rooms and corridors. Hospital-grade vinyl would replace fabric on furniture. Curtains would be replaced with motorized shade systems. Mobile headwall units and portable med gas bottles would be installed, as would electronic wireless patient surveillance and monitoring devices. The converted hotel would also need to create storage areas for portable medical equipment. (Medical gases would have to be portable.)
Reuse Model 3 would require all of the modifications described in Reuse Models 1 and 2. Leo A Daly suggests that exhaust modifications may not be necessary in all rooms. But infrastructure changes would include providing an exterior emergency generator system and transfer switch equipment for connection to the building’s power infrastructure. The IT infrastructure would be upgraded. Treatment and procedure spaces would be identified and equipped with recirculating HEPA filtration units to increase the room’s air changes per hour.
Theodore acknowledges that the Hotel2Hospital prototype conversions would need to address challenges that include staffing, HVAC, building codes, medical equipment management, the building’s power infrastructure, and meeting cleaning/support standards.
He says that Leo A Daly’s design teams have been meeting with hospitals, federal officials, developers and hotel owners to work through these complexities
Related Stories
Coronavirus | Jun 14, 2020
A new report on how campus buildings can reopen safely
Leo A Daly white paper suggests dividing students into smaller “cohorts,” and assigning bathroom spaces.
Coronavirus | Jun 12, 2020
BD+C launches 'The Weekly,' a streaming program for the design and construction industry
The first episode, now available on demand, features experts from Robins & Morton, Gensler, and FMI on the current state of the AEC market.
Coronavirus | Jun 9, 2020
Going viral: How the coronavirus pandemic could change the built environment
Architecture and construction firms—and their clients—are asking new questions about infection control as it pertains to people assembly, building wellness, and technology.
Fire and Life Safety | Jun 9, 2020
NFPA develops business reopening checklist for fire and life safety measures
The new checklist helps building owners and facility managers ensure fire and life safety as businesses prepare to re-open amid the coronavirus pandemic.
Coronavirus | Jun 9, 2020
CannonDesign unveils COVID Shield
As the world evolves its response to the COVID-19 pandemic, one clear reality is testing for the virus will be part of our daily lives for the foreseeable future.
Coronavirus | Jun 5, 2020
3 strategies to improve the wellness of building systems and gain tenant trust
Three operational issues that must be prioritized for every building in order to achieve tenant trust are air quality/ventilation, relative humidity, and building commissioning.
Coronavirus | Jun 2, 2020
5 ways to improve hand washing and minimize germs in public restrooms
Bradley Corp. offers five upgrades to make public restrooms more sanitary.
Coronavirus | Jun 2, 2020
Perkins and Will, Healthy Building Network advise against the use of antimicrobial building products
Even during a pandemic, antimicrobial building products may do more harm than good.
Coronavirus | May 30, 2020
A welcoming entry-point for wellness screening anywhere
Modular WorkWell™ ecosystem can process up to 40 people per minute.
Coronavirus | May 29, 2020
Black & Veatch, DPR, Haskell, McCarthy launch COVID-19 construction safety coalition
The NEXT Coalition will challenge engineering and construction firms to enhance health and safety amid the Coronavirus pandemic.