Healthcare consumers are just as likely to factor in convenience as they do cost when deciding where to seek care and from whom, according to a new survey of 4,037 American adults about their attitudes and preferences as patients.
The survey, conducted from April 19-28 by JLL, in many ways confirms the obvious: that older generations seek preventive care more often than younger generations; that insurance coverage is a primary driver for choosing a provider or hospital; and that the quality of service affects the patient experience.
Nearly eight of 10 of the survey’s respondents had received at least one type of non-dental care in the last year. Women, who accounted for 51% of the survey’s respondents, are more likely to receive care overall, but men are more likely to receive emergency care.
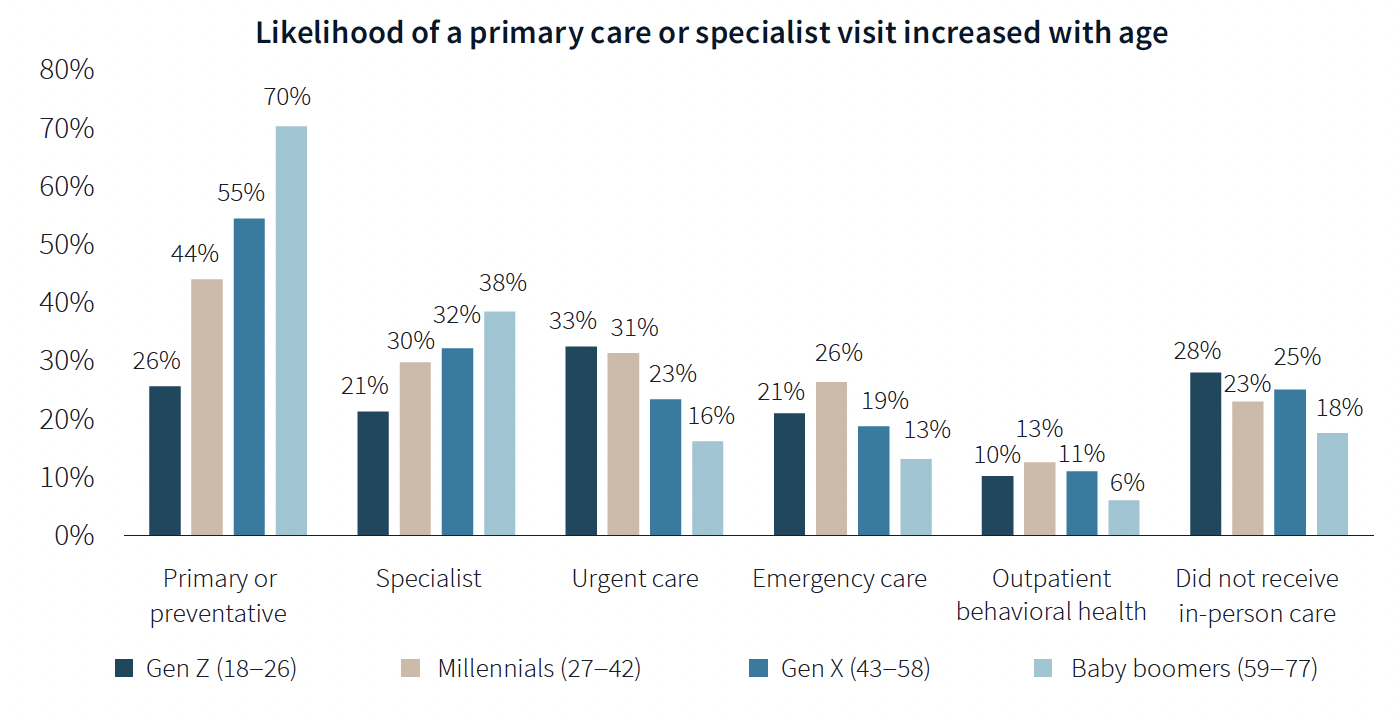
The likelihood of a primary care or specialist visit increases with age: 80% of adults 65 years or older have two or more chronic conditions that require continuous care. More than 70% of Baby Boomers (who accounted for 29% of the survey’s respondents) had received primary or preventive care within the last year, compared to only 26% of Generation Z.
Younger generations are more reactive than preventive in their healthcare decisions, borne out by the survey’s finding that Millennials and Gen Zs (43% of the survey's respondents) are more likely to receive urgent care, emergency care, and outpatient behavioral healthcare than older adults.
Proximity to patients counts
When care is urgently needed, “decision factors are simplified,” the survey states, and location and proximity of care are ranked higher as decision-making factors. But even outside of emergencies, convenience ranks high among factors for patients seeking care.
There’s no denying that cost is always in the background of any healthcare decision. “Accept my insurance” was the most common factor for choosing a provider among the survey’s respondents. (82% of participants has private insurance, and 81% has public insurance.)
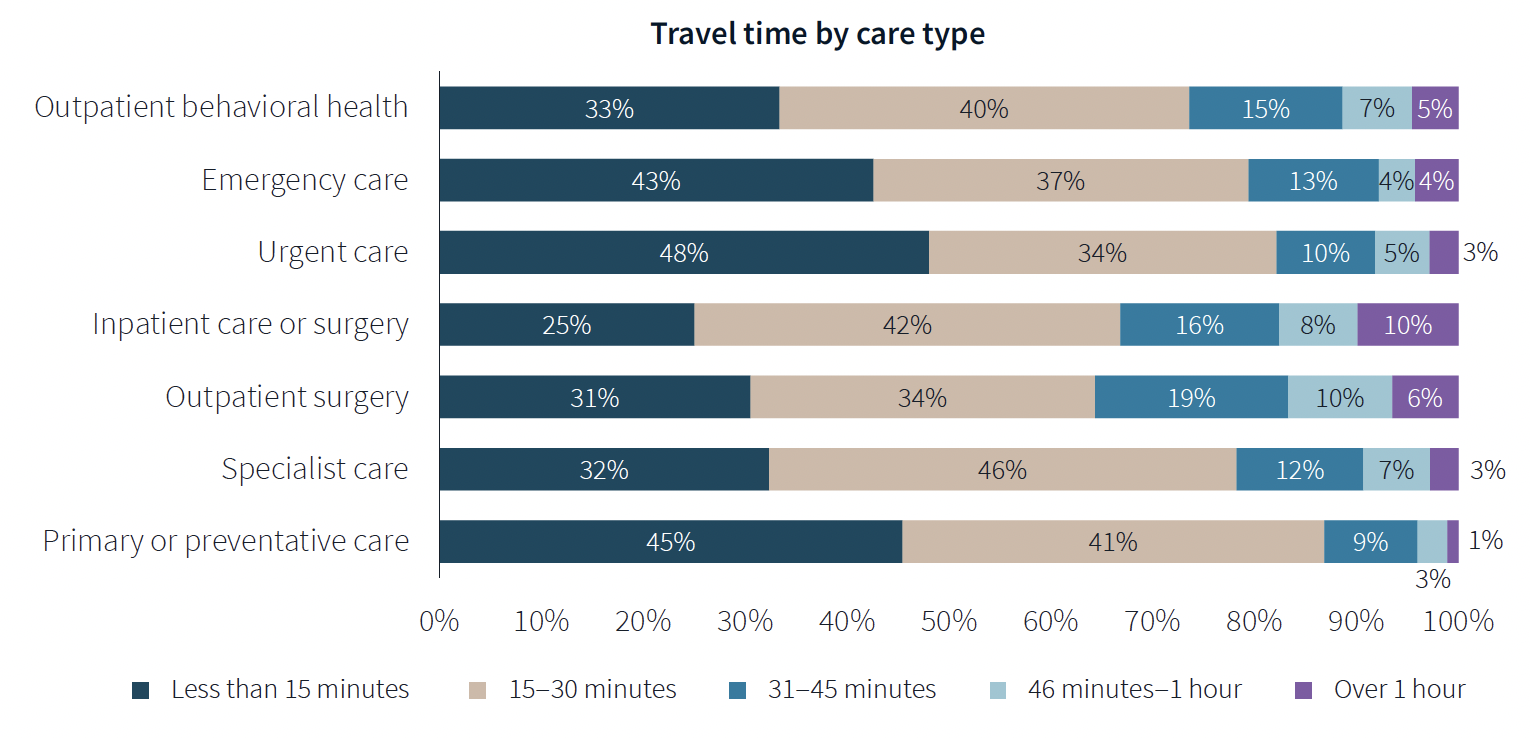
Two-fifths of respondents said they travel less than 15 minutes to receive care, and nearly eight of 10 respondents travel less than 30 minutes. Among those with appointments in standalone medical offices, 85% ranked location as convenience, which the survey suggested indicates the advantages of a dispersed location strategy.
“A strong location strategy can improve reach for health systems and physician practices and potentially improve care outcomes,” JLL writes. “But there is a balance between convenience and cost—health systems need to balance the benefits of being close to their target population with the cost of a new facility or doctors’ time in transit from a local clinic to the hospital.”
Convenience is also key both in location and in being able to navigate to care. Patients want to get to care quickly and get on with their day. Ease of parking and ability to navigate the facility also affected a facility’s net positive score in the survey.
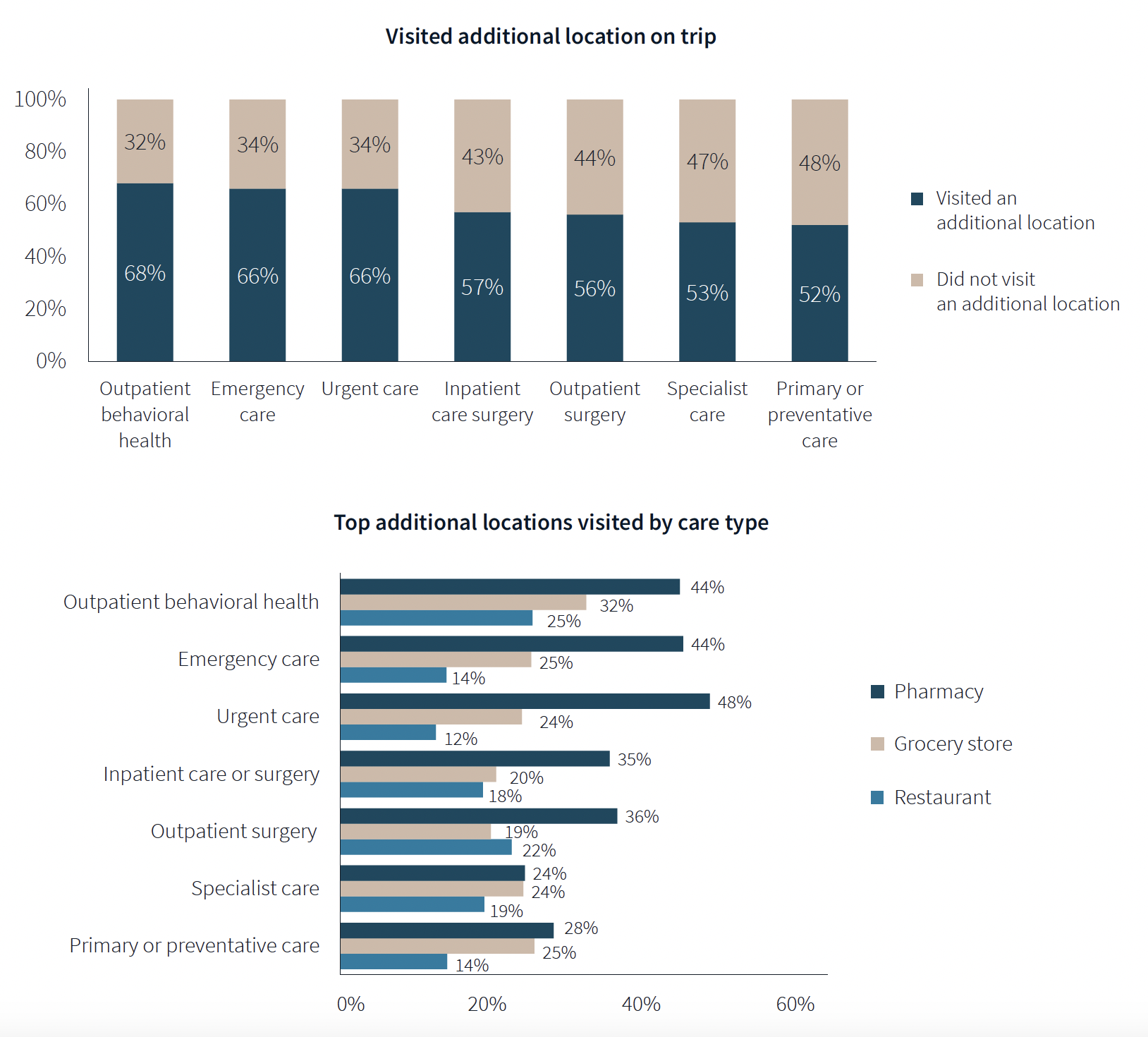
One of the survey’s more revealing findings is that nearly three-fifths of respondents—58%—went to another location—such as a pharmacy, or an urgent clinic—as part of their trip for healthcare.
Word of mouth often defines quality of care
Patients seem to be open to diverse care choices. For example, 29% said they have visited a retail clinic, such as a CVS, and would do so again. Gen Z and Millennials are more likely to frequent retail clinics for their convenient appointment schedules and shorter wait times.
More than two-fifths of respondents—42%—had a telehealth appointment within the last year, which was slightly down from the 45% in JLL’s 2022 survey. This year’s poll also found that 29% of telehealth appointments led to an in-person visit.
More than 40% of respondents ranked “reputation of quality” among the top five factors for choosing care. But where they get their impressions about quality varies.
Referrals play a larger role in specialist, outpatient surgery and inpatient care. Recommendations from friends ranked most highly for behavioral health, given the personal nature of such care, and was ranked in the top five by 31% of respondents. Younger patients, who “have yet to develop brand loyalty,” according to the survey, are more likely to rely on word-of-mouth recommendations than older patients for whom hospital systems’ reps matter more.
Outpatient surgery and primary care ranked highest for provider satisfaction; emergency care ranked lowest. Participants ranked their experiences on 12 aspects of care, and the biggest gap between “promoters” and “detractors” was for the service level of providers. Primary care had the highest net provider score, with 86% of respondents ranking its care as “attentive.”
Some amenities draw patients
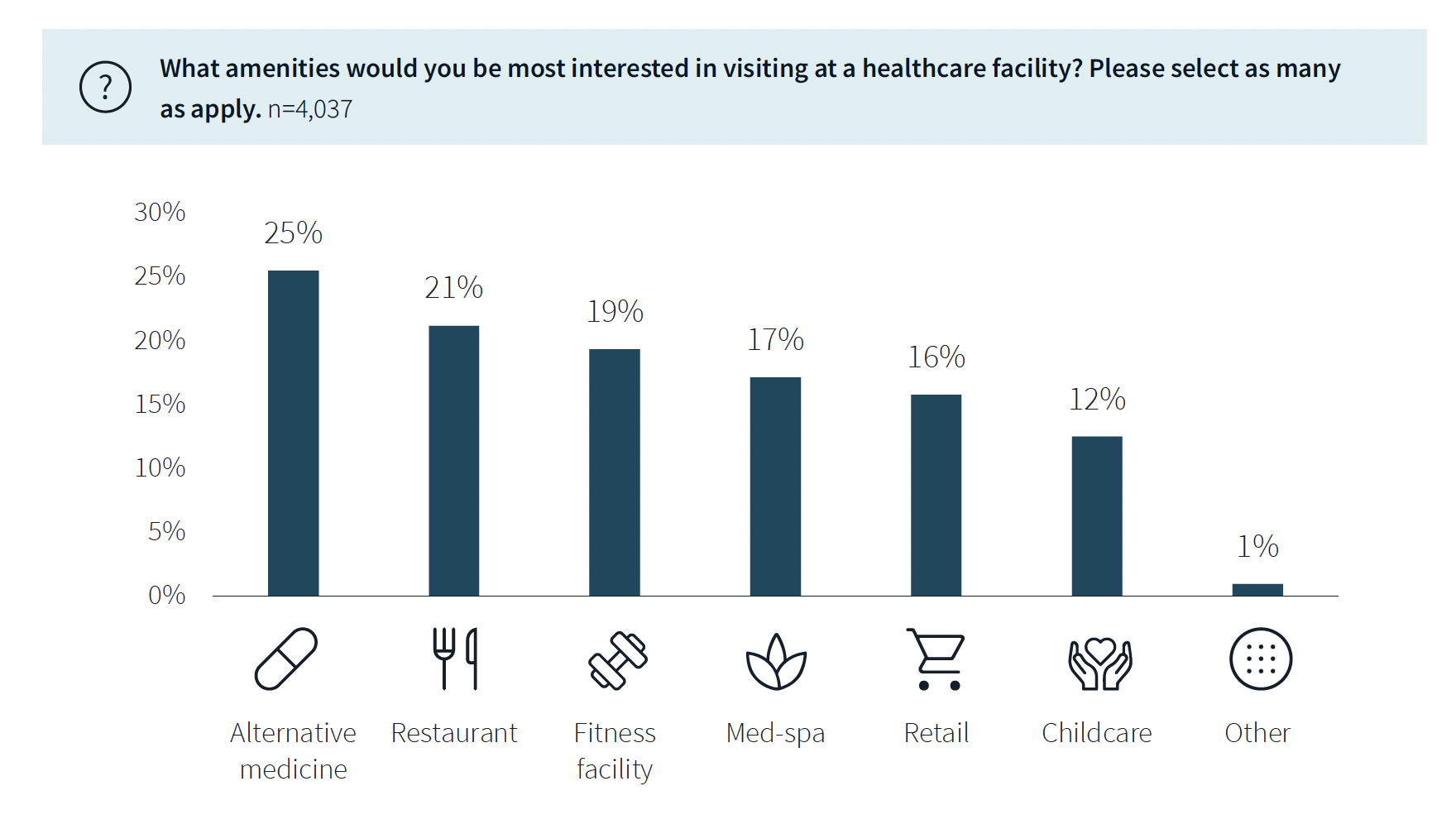
While not a decision-making factor, amenities do attract some patients. Among the survey’s respondents, 63% said they would be interested in visiting a healthcare facility with an additional amenity, such as alternative medicine, a restaurant, fitness center, or spa. (This inclination was more evident among younger respondents.)
The overall quality of facilities, including the comfort of their waiting rooms, can impact a patient’s choice, especially for inpatient, urgent, and emergency care. The survey also found that urban locations have lower favorability rankings for their facilities, signaling room for improvement. (Just under half—48%—of respondents live in the suburbs.)
Related Stories
Healthcare Facilities | Dec 29, 2015
Wood materials aid in patient recovery in healthcare environments
Report says patient recovery times, pain perception, stress levels improve where natural materials are present.
Healthcare Facilities | Dec 15, 2015
What the Bipartisan Budget Act of 2015 means for healthcare real estate development
CBRE Healthcare's Charles Maggio breaks down the impacts of the new legislation, which affects outpatient facilities.
Greenbuild Report | Dec 10, 2015
Sustainable performance: Hospital systems’ new financial and marketing imperative
Several years ago, the healthcare industry would have ranked in the bottom tier among adopters of sustainable design and construction. Now, it is outpacing other nonresidential sectors in moving toward high-performance, healthy environments.
Healthcare Facilities | Dec 2, 2015
Check out Perkins+Will’s ultra-transparent research center for the Allen Institute for Brain Science
The design orients labs like flower petals around a large light-filled central atrium; the effect is like the inside of a bee hive where researchers can see each other and what they are doing.
Healthcare Facilities | Nov 6, 2015
Paint company unveils product that can kill bacteria in hospitals
The new product from Sherwin-Williams, called Paint Shield, is said to not only kill over 99.9% of dangerous bacteria, but also reduces growth of “common microbes.”
Healthcare Facilities | Nov 4, 2015
Hospital designers get the scoop on the role of innovation in healthcare
“Innovation” was the byword as 175 healthcare designers gathered in Chicago for the American College of Healthcare Architects/AIA Academy of Architecture for Health Summer Leadership Summit.
Healthcare Facilities | Nov 2, 2015
Final funding comes through to complete over-budget and behind-schedule Denver VA Medical Center
The Department of Veterans Affairs, cited for its mismanagement, is stripped of control over future major construction.
Healthcare Facilities | Oct 23, 2015
Mortenson study: Healthcare providers optimistic, but want changes to Affordable Care Act
The 2015 Mortenson Healthcare Industry Study found that 76% of providers are at least optimistic about the future of healthcare, but eight out of 10 would like to see changes made to ACA.
Healthcare Facilities | Sep 29, 2015
The ever changing physician real estate market
In the United States, the environment where outpatient healthcare is being delivered is as dynamic and diverse as the more high profile office and retail markets, writes CBRE Healthcare's Nelson Udstuen.
Healthcare Facilities | Sep 21, 2015
5 reasons healthcare organizations are implementing finish standards on construction projects
The desire for improved patient satisfaction, staff retention, and turn-key maintenance are among the top reasons more healthcare groups are implementing finish standards in their spaces, according to VOA Associates' Lauren Andrysiak.

















