Hospitals across the U.S. are already heavily burdened during flu season, with some operating at 110% capacity during its peak. COVID-19 adds stress to an already taxed system, threatening bed shortages and staffing issues.
Coronavirus patients also bring the risk of infection for healthcare workers and patients with other serious ailments when they enter a hospital. Meanwhile, only the most acutely ill COVID-19 patients need hospitalization. (Mild cases are encouraged to self-isolate in their residence.)
We have seen mortality rates from COVID-19 spike when health systems become exhausted, such as in Milan and Wuhan. As U.S. healthcare administrators consider outside-the-box solutions to expanding capacity, here are some thoughts to consider from a design perspective.
Look at hotels
Freeing up beds for the most acute patients is critical as COVID-19 spreads. As more patient hit the emergency department looking for care, difficult decisions will need to be made about who stays and who goes home. Severely acute patients without the virus will still need ICU beds. Some COVID-19 patients will require acute care, while many more will need to be quarantined.
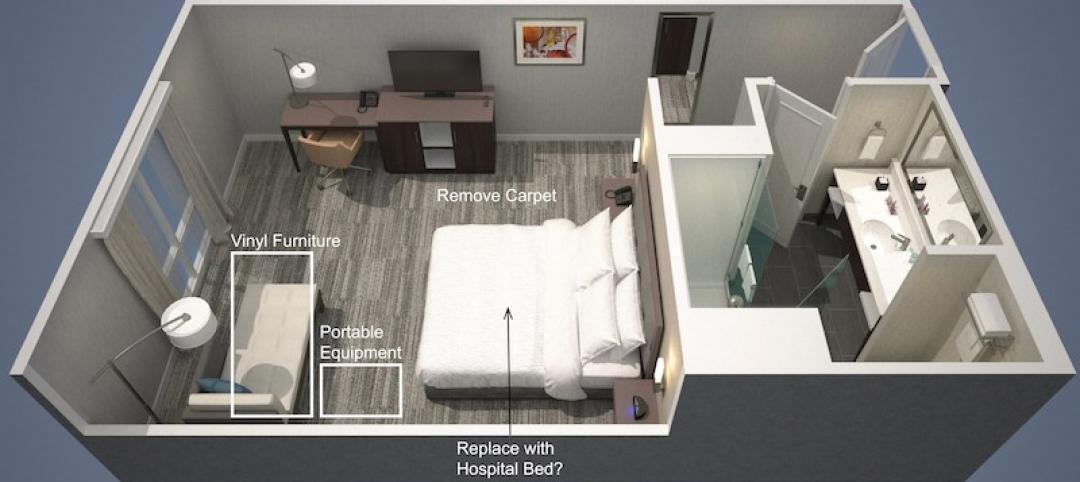
Hotels are well situated to transform quickly into pop-up quarantines, and they have an economic incentive to do so as bookings have temporarily dried up. Several features make hotels easy to convert. They are made of private, individual rooms with dedicated toilets and HVAC. Their facilities already offer food service, cleaning services, waste removal and laundry. They are secure and many are located near existing hospitals.
The LEO A DALY healthcare team has already begun working with some developers on plans to retrofit hotels as COVID-19 quarantines. Minimal modifications to the rooms will be required. Nurse stations will be added to each floor. Reception desks will become patient check-in areas; retail areas will become pop-up pharmacies; offices will become labs. Exhaust fans added to roof ducts will create negative pressure rooms. Et voila – a pop-up isolation facility.
Add anterooms to existing isolation units
Major construction projects within operational hospitals are unlikely to begin during the current epidemic, and many counties have shut down all construction sites as a social distancing measure. Still, in a pinch, a relatively small intervention could transform any existing patient room floor into an isolation ICU.
Our healthcare teams have discussed surgically adding anterooms to the entrances of non-ICU hospital wings, creating an air lock that would isolate airborne pathogens within the wing. Patients within the unit would still potentially be infectious to each other, and staff would have to observe strict PPE protocols, but the adjacent hospital areas would be free from contamination and able to continue serving non-COVID-19 patients.
Leverage disused or underutilized facilities
With many ambulatory surgery centers cancelling elective procedures, there is an opportunity to convert them temporarily into acute COVID-19 treatment centers. Although they do not have the same containment capabilities as an ICU, they are set up to deliver round-the-clock medical care in an isolated environment.
Right now, we have not seen the level of cooperation among the independent owners of ambulatory centers and the larger health systems that handle the bulk of acute care. Collaboration would be necessary in order to leverage these facilities to fight COVID-19. In the absence of a singular, national healthcare system in the U.S., this is unlikely. However, something like an Executive Order could be used to mandate cooperation.
Social distancing and shutdowns of college campuses are now prevalent, making dormitories basically empty. These could be used for quarantine, for isolation (with HVAC changes), or to house otherwise healthy hospital patients that can’t quite go home. Most modern student housing is now built with en suite toilets, which would be an important amenity for patients. Leveraging student housing would increase the capacity of the whole healthcare system.
Many more underutilized facility types could be used for surge capacity. Low-occupancy post-acute care facilities and empty nursing homes could be a fit for quarantine of asymptomatic patients.
These are just a few ideas for responding to the shortage of acute care beds that experts anticipate as COVID-19 grows. Any of them will require healthcare administrators, lawmakers, developers and others to think outside the box and embrace innovative solutions. Code requirements may also need to be relaxed for interim measures. With all states under a State of Emergency, Governors would have the ability to enact interim measures allowing for more rapid deployment.
At this unprecedented time of crisis, design thinking and collaboration will be some of our strongest tools in the fight against infectious disease.
Related Stories
Coronavirus | Apr 1, 2020
TLC’s Michael Sheerin offers guidance on ventilation in COVID-19 healthcare settings
Ventilation engineering guidance for COVID-19 patient rooms
Coronavirus | Apr 1, 2020
February rise in construction outlays contrasts with pandemic-driven collapse in March as owners, government orders shut down projects
Survey finds contractors face shortages of materials and workers, delivery delays and cancellations.
Coronavirus | Apr 1, 2020
Green cleaning and the coronavirus
If your cleaning teams use bleach to disinfect buildings from Coronavirus, will you put your LEED certification at risk?
Coronavirus | Mar 31, 2020
As cities scramble for hospital beds to treat COVID-19 patients, Leo A Daly offers a hotel-to-hospital solution
The firm has devised three conversion models, for different levels of healthcare required.
Coronavirus | Mar 30, 2020
Your turn: Has COVID-19 spelled the death knell for open-plan offices?
COVID-19 has designers worrying if open-plan offices are safe for workers.
Coronavirus | Mar 30, 2020
Learning from covid-19: Campuses are poised to help students be happier
Overcoming isolation isn’t just about the technological face to face, it is about finding meaningful connection and “togetherness”.
Coronavirus | Mar 30, 2020
COVID-19 innovation: Setting parameters for hotel-to-hospital conversions
tvsdesign breaks down different room types and how they might help free up hospital beds for coronavirus patients.
Coronavirus | Mar 30, 2020
New Department of Homeland Security guidance clarifies construction's role in supporting essential critical infrastructure
Construction officials say new federal guidance should signal to state and local officials the need to allow construction activity to continue, or resume, during coronavirus-related work stoppages.
Coronavirus | Mar 27, 2020
Sharp jump in owners cancelling or delaying construction projects across the country, new survey finds
After 42 states added jobs in February, coronavirus is taking a swift and severe toll on the industry, prompting association officials to call for additional measures to help workers and firms recover.
Coronavirus | Mar 27, 2020
Covid-19 stalls demand for design services
Two thirds of architecture firms report slowing or stoppage of projects due to COVID-19.