The built environment has a profound impact on our natural environment, economy, health, and productivity, according to the US Green Building Council (USGBC). In the United States alone, buildings account for:
* 65% of electricity consumption
* 36% of energy use
* 40% of greenhouse gas emissions
* 30% of raw materials use
* 30% of waste output (136 million tons annually)
* 12% of potable water consumption
When you think about these statistics, it’s no wonder that a movement toward sustainability has been underway for the past 16 years. LEED (Leadership in Energy and Environmental Design), first introduced in 2000, is an ecology-oriented building certification program run under the auspices of the USGBC. LEED concentrates its efforts on improving performance across five key areas of environmental and human health: energy efficiency, indoor environmental quality, materials selection, sustainable site development and water savings.
The LEED rating is the globally accepted benchmark for the design, construction, and operation of high-performance green buildings. LEED certification provides independent, third-party verification that a building project is environmentally responsible and a healthy place to live and work.
Early adopters in the healthcare sector struggled with adapting LEED standards to the special needs of healthcare operations with limited success. Recognizing this, in 2009 the USGBC launched LEED for Healthcare, codifying in the LEED structure principles from the Green Guide for Healthcare. In 2011, LEED for Healthcare was updated and rebranded as LEED BD+C: Healthcare. This designation seeks to align the points of emphasis from the traditional LEED framework to the realities of the healthcare environment. For example, many of LEED’s Indoor Environmental Quality requirements were modified to reflect the need for infection prevention, as well as the existing code requirements for ventilation in healthcare facilities. Since its launch, over 40 different projects worldwide have met LEED criteria to be certified by the USGBC under LEED for Healthcare.
The pursuit of LEED can come with a price tag, in some cases adding a 1% to 3% premium to the overall construction budget. With tight budget constraints placed on healthcare executives, paying the additional premium to be “green” and achieving the project’s financial goals can be seen as mutually exclusive. However, when considering the triple bottom line—Pocketbook, People, and Planet—going green can be a responsible decision.
Pocketbook
Energy costs represent a large portion of healthcare expenditures. Recognizing this, over one fifth of the available LEED points are tied to energy performance gains. At a minimum, LEED requires a 10% improvement in building performance rating over the baseline case. Initially, achieving these credits can be costly. However, a payback in energy savings can be realized down the road. For example, high-efficiency chillers can cost 20% more than comparable standard units, but installing these more efficient units can result in up to a 42% reduction in the energy required for space cooling and a potential 48% savings in cooling tower use.
In addition, process water used to operate building systems such as boilers, chillers, cooling towers, and sterilizers comprises 75% of the water used at hospitals. Even modest improvements in process water efficiency (e.g. using condensate for cooling tower makeup water) can save institutions thousands of gallons of water annually.
Lighting upgrades, coupled with smart controls and increased natural lighting, can decrease electrical usage while creating an environment more conducive to healing. Recent advances in LED lighting technology have in many instances made the first cost of these fixtures equal to or less expensive than fluorescent or incandescent options.
People
Increasing connections to the natural environment and available natural light are important components of the LEED framework. A growing body of research shows positive correlation between maximizing natural light and reduced lengths of stay. Prudent owners are requesting that their designers go well beyond the code minimum requirements for clear views in order to take advantage of this correlation.
Giving patients control over their environment has been linked with better patient outcomes and higher patient satisfaction scores. Dimmable lighting systems, operable window shades, and in-room thermostats allow the in-room environment to be tailored to the particular needs of each patient. Coupled with a robust building automation system, these control points can also be used to reduce energy consumption by avoiding unnecessarily lighting or heating unoccupied spaces.
Building green can also increase staff satisfaction. Recent studies have shown a link between LEED facilities, staff comfort, and satisfaction levels. For example, a 2014 study in the Journal of Hospital Administration showed higher levels of staff engagement at the LEED Platinum Dell Children’s Hospital in Austin, Texas, compared to two other non-LEED hospitals. In addition, staff turnover decreased after moving from Dell’s predecessor into the new LEED facility.
Better indoor air quality-that is, the control of both internally generated and external pollutants-will also have a positive impact on the well-being of building occupants. Careful selection of building materials, along with proper ventilation, operation, and maintenance can improve indoor air quality. Improvements in the indoor environment of our healthcare facilities can have a profound impact on sensitive populations such as children, the elderly, and patients who are immunocompromised or have respiratory problems.
Planet
In 2009, researchers estimated that greenhouse gas emissions related to healthcare activities represented 8% of the total in the United States. More recent research has shown that the healthcare sector’s carbon footprint is growing, increasing by more than 30% over the past 10 years.
Greening both the built environment and the supply chain provides hospitals the opportunity to live up to their obligation to “first, do no harm.” By making environmentally conscious choices in the design and construction of their facilities, organizations can reduce their impact to the planet. As noted above, reduction in energy and water usage will show up on financial statements, but in considering the decision to go green administrators should weigh such non-financial measures as:
* waste diverted from landfills
* reduction in water drawn from aquifers
* reduction in wastewater discharged to local waterways
* reduction in carbon emissions from power plants, boilers, and generators
* access to green transit options, which lower the environmental impacts of staff and patient commuting
* use of sustainable building materials and products
Conclusion
As we approach the end of the second decade of LEED, the financial costs and benefits of going green are well documented. In many cases, due to increased demand for environmentally friendly products, the cost of implementing certain green strategies is negligible. However, there are still areas where green choices do not pass a purely financial test.
Fortunately, healthcare systems are not purely in the business of generating financial returns. Healthcare organizations must also care for people they encounter—patients, staff, and visitors—and the world around them. Considering the triple bottom line, pocketbook, people, and planet, gives healthcare executives additional justification for using green building strategies to advance the organization’s mission.
Related Stories
Healthcare Facilities | Apr 13, 2017
The rise of human performance facilities
A new medical facility in Chicago focuses on sustaining its customers’ human performance.
Healthcare Facilities | Apr 11, 2017
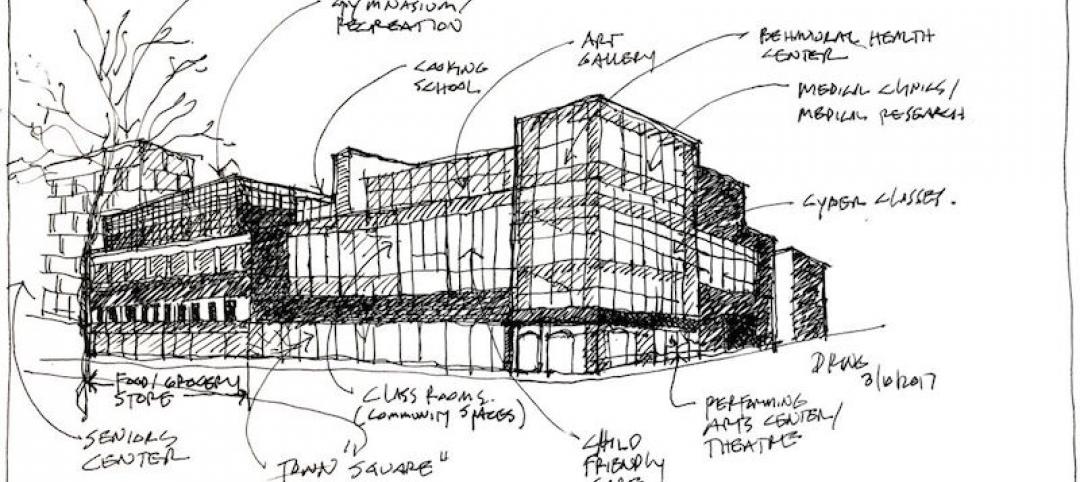
Today’s community centers offer glimpses of the healthy living centers of tomorrow
Creating healthier populations through local community health centers.
Healthcare Facilities | Apr 2, 2017
Comfort and durability were central to the design and expansion of a homeless clinic in Houston
For this adaptive reuse of an old union hall, the Building Team made the best of tight quarters.
Healthcare Facilities | Mar 31, 2017
The cost of activating a new facility
Understanding the costs specifically related to activation is one of the keys to successfully occupying the new space you’ve worked so hard to create.
Sponsored | Healthcare Facilities | Mar 29, 2017
Using Better Light for Better Healthcare
Proper lighting can improve staff productivity, patient healing, and the use of space in healthcare facilities
Healthcare Facilities | Mar 29, 2017
Obamacare to Republicare: Making sense of the chaos in healthcare
With a long road of political and financial uncertainty ahead for the healthcare sector, what does this mean for the nonresidential construction industry’s third-largest sector?
Healthcare Facilities | Mar 24, 2017
5 insights for designing a human-centered pediatric experience
Pediatric experience design must evolve beyond the common mantra of “make it fun” or “make it look kid-friendly.”
Healthcare Facilities | Mar 3, 2017
CBRE: Developing a total project budget for a healthcare capital project
Successfully developing a complete and well thought out Total Project Budget is perhaps the most important task you’ll perform in the initial phase of your project.
Healthcare Facilities | Feb 26, 2017
A Georgia Tech white paper examines the pros and cons of different delivery systems for ICUs
It concludes that a ceiling-mounted beam system is best suited to provide critical care settings with easier access to patients, gases, and equipment.
Healthcare Facilities | Feb 24, 2017
The transformation of outpatient healthcare design
Higher costs and low occupancy rates have forced healthcare facilities to rethink how healthcare is delivered in their community.