Editor's note: This article was originally published as part of BD+C's two-part March 2014 Healthcare Facilities Report. Read the second installment of the report, "6 keys to better healthcare design."
Recent efforts to curb healthcare spending by the federal government and insurers appear to be working, something most Americans would say is a good thing—unless, of course, you’re the poor healthcare property management executive at a struggling healthcare provider.
Total U.S. spending on healthcare grew 3.7% in 2012, marking the fourth straight year of “low growth,” according to the Centers for Medicare & Medicaid Services (CMS). This compares with annual increases as high as 16% in past years, according to the CMS, which has been tracking healthcare costs since the 1960s.
According to the American Hospital Association:
• Medicare and Medicaid payments to hospitals have been cut by an estimated $113 billion since 2010.
• Underpayment by Medicare and Medicaid to U.S. hospitals reached $56 billion in 2012.
• U.S. hospitals provided $45.9 billion in uncompensated care in 2012.
Revenue projection is critical to capital expenditure planning, and uncertainty over how the Affordable Care Act will impact hospital reimbursements only adds to the complexity of the problem. If the law helps enough people get insurance, hospitals could get paid for care they now provide free to the uninsured. On the other hand, the ACA could send a flood of previously uninsured patients seeking expensive treatments that could strain capacity.
5 Tips For Winning More Healthcare Work
TIP 1 - "We want the people who are handling our work to have some clout within the firm. If something unexpected happens and we need an all-out effort, we want people who can go to leadership and get resources committed. We also like firms that are able to devote resources to healthcare design research."
— Bob McCoole, Senior Vice President, Facilities Resource Group, Ascension Health
TIP 2 - “During interviews, we only allow those directly involved in the project in the room. We don’t allow principals or marketing people—only PMs and superintendents. We don’t want marketing people trying to dazzle us. We also look for a good track record on safety and disruption avoidance.”
— John A. Balzer, MSEM, Vice President, Facility Planning and Development, Froedtert & the Medical College of Wisconsin
TIP 3 - “When making a proposal, we like to see firms that understand the market at the campus, our competition, and the history and layout of the campus.”
— Jim Young, Director, Capital Project Management, CHE Trinity Health
TIP 4 - “Part of engaging well in the IPD process is having an enculturation of collaboration. Some firms and individuals don’t seem to have that, but over time, the number of firms that we are excusing from projects for that reason is shrinking.”
— Carl Scheuerman, FACHE, Director of Regulatory Affairs, Sutter Health
TIP 5 - “Architects need to keep their egos in check, be open-minded, and understand that there are going to be a whole lot more people developing the drawings than themselves. We have a draw-once strategy. We didn’t want to recreate drawings. Architects and fabricators sat side by side. Electricians and mechanics worked together as team.”
— Paul Stein, Chief Operating Officer, MaineGeneral Medical Center
Furthermore, the underlying goal of the ACA is to reward hospitals for improving quality of care, rather than paying providers for services no matter what the outcome for patients. Then there are the penalties. Last year, hospitals with readmission rates considered excessive began having their reimbursement rates trimmed. Next year, hospitals with high rates of hospital-acquired infections will start seeing their reimbursement rates cut even more severely. All this makes accurate forecasting of hospital space needs no better than semi-educated guesswork.
In a year or two, the reimbursement picture should become clearer. For now, healthcare facility planners can count on two things: 1) they need to help rein in costs as much as possible, particularly through greater efficiency, and 2) they need to do everything they can to improve patient outcomes.
To get a boots-on-the-ground perspective, Building Design+Construction asked seven top healthcare industry capital planning executives for their views on how the upheaval in healthcare impacts capital planning, new construction, and renovations. Thought their institutions share some common coping strategies, each has different areas of emphasis. But there’s one thing all our experts agreed on: Capital is in short supply and is likely to get even tighter this year.
ASCENSION HEALTH: THE BUMPY ROAD TO OUTPATIENT SERVICES
Ascension Health is the nation’s largest Catholic and largest nonprofit healthcare system, with 1,500 locations in 23 states. For Ascension, the migration to same-day surgeries and procedures hovers like a specter over the organization’s facility planning.
“Everybody knows we as an industry need to move from the inpatient model to more of an outpatient model, but that doesn’t mean there is going to be a flood of capital available,” says Bob McCoole, who oversees Ascension’s facilities. Given the pressures to improve services on tighter budgets, McCoole sees a need for fundamental change in healthcare design. “If the facilities we design today look like what’s been built before, we’re not accomplishing anything,” he says.
“We are scouring opportunities to lower costs in every area of the business,” says McCoole. McCoole and Ascension executives are striving to identify the appropriate level of contribution to cost reduction by the physical plant. On average, facilities account for 8-12% of overall healthcare expenditures, he points out, and there are several areas ripe for cost cutting.
At the top of the agenda: a systemwide review of all properties in order to consolidate facilities. Ascension has hired a real estate consulting firm to pore through its entire portfolio—hospitals, ambulatory centers, and medical offices—for consolidation opportunities. The consultant will also be looking to “comb leases for accuracy of terms” and to assess maintenance costs.
Also on tap: energy-efficiency retrofits, further development of design standards, and a review of the organization’s preferred design firm list for projects of more than $10 million.
CHE TRINITY HEALTH: CONSOLIDATING TO COMPETE
Last May, Trinity Health merged with Catholic Health East, creating CHE Trinity Health, one of the nation’s largest Catholic healthcare systems. It has a presence in 20 states with 82 hospitals, 88 continuing care facilities, and home health and hospice programs.
The newly minted merger presents Jim Young, Capital Project Management Director, with the task of bringing the two cultures together. “Legacy Trinity,” as Young calls the pre-merger entity, “had a more centralized approach to capital project management and real estate.” Updating design standards for the merged organization is being looked at as a means to control costs, with a focus on stabilizing room size and expenditures on aesthetics.

Ascension Health’s 155,395-gsf, 64-bed St. Vincent’s HealthCare hospital, in Jacksonville, Fla. Building Team: HKS (architect), UHS Building Solutions (design-build firm), TLC Engineering for Architecture (MEP), Prosser Hallock (CE), TME Inc. (commissioning engineer), Miller Electric Co., W.W. Gay Mechanical Contractor, HBS Healthcare Building Solutions, and Brasfield & Gorrie (GC). The three-story tower has six ORs, 32 med/surg beds (orthopedics and neurology), a 24-bed general medical surgical floor, an eight-bed ICU, a 16-bay ED, a catheterization lab, and a check-in kiosk with palm scanner. Photo: Lans Stout
As much as cost cutting seems the right way to go, market forces also have to be plugged into the equation. “We’re in some very competitive markets where the state of competitors’ facilities is often at a high level,” says Young. “People interpret facility quality and appearance as an aspect of good healthcare.” So there is pressure to stay on par with what competitors are building where supported by a strong business case.
Another focus is energy savings upgrades, as well as an effort to boost efficiency on major renovations and new construction by using commissioning agents early in projects. Young says commissioning has already proven its worth on CHE Trinity projects.
SUTTER HEALTH: WINDING DOWN THE seismic SPENDING SPREE
Sutter Health serves more than 100 communities in Northern California with 21 hospitals and medical centers. The organization is in the latter stages of a huge construction program to comply with the California Hospital Seismic Safety Act, which was enacted in the wake of the deadly 1994 Northridge earthquake.
“The Act pushed us a little bit further into the future than maybe we wanted,” says Carl Scheuerman, FACHE, Sutter’s Director of Regulatory Affairs. The law, which mandated stiff requirements for seismic resilience in hospital retrofits or new construction, pushed California hospitals to the forefront of the inpatient-to-outpatient trend. According to Scheuerman, “At the onset, the big question was should we take half-measures to retrofit buildings, or make major investments in new buildings?” It was determined that, in most cases, retrofits would merely have extended the life of outdated facilities at a high cost, so new construction was usually the chosen path.
With the hospital building spree winding down, “The lion’s share of capital is going to be spent on the ambulatory environment,” says Sutter Health’s Planning and Design Chief, Dan Conwell. Many of these projects will be for small, highly focused services often located in strip malls. Sutter will also roll out more “express care clinics” in supermarkets or drugstores to provide low-cost services closer to the customer.
MAINEGENERAL: FINDING EFFICIENCIES EVERYWHERE
When MaineGeneral’s new Alfond Center for Health opened last November, it more than doubled the inpatient capacity of the organization’s two existing hospitals. One of those facilities, the Thayer Center for Health, is undergoing a major renovation and conversion to an emergency and outpatient facility. The $322 million being spent on these two projects represents a once-in-a-lifetime opportunity to remake this small healthcare system centered in the capital city of Augusta.

Sutter Health Eden Medical Center, Castro Valley, Calif. The 220,000-sf, 130-bed acute care facility was completed through an 11-party IPD agreement led by DPR Construction, with architect Devenney Group. The hospital has a 22-bed emergency department and a 34-bed universal care center. Rien Van Rijthoven
In Yankee tradition, the organization carefully measured how every dollar would be spent. “Where do we spend to get efficiencies and return on investment?” says COO Paul Stein. “We have one chance to do this, so we better get it right.”
Many stakeholders were involved in the planning for the Alfond Center—medical and non-medical staff, facilities/maintenance personnel, a Patient Family Advisory Council, and the hospital’s Lean process team, which is composed of four highly trained specialists who focus on analyzing hospital processes, recommending ways to improve efficiency, and training staff on how to implement those improvements. The Lean process team also contributes to the design of interior spaces, particularly in influencing layout standards and features that impact the flow of patients, physicians, and staff.
FROEDTERT & MEDICAL COLLEGE OF WISCONSIN: ‘RIGHT CARE, RIGHT PLACE, RIGHT TIME’
Froedtert & the Medical College of Wisconsin, centered in Milwaukee, is a regional healthcare network made up of three hospitals and more than 30 primary and specialty care health centers and clinics. The 500-bed Froedtert, the region’s only teaching hospital, is located on prime real estate in downtown Milwaukee.
Capital planning for the hospital is guiding by the principle that downtown space should house the highest-value services. For example, a current project to relocate some orthopedic services from the downtown campus will free up space for higher-end procedures such as organ transplants and cardiovascular care, says John A. Balzer, MSEM, Vice President of Facility Planning and Development. “Just as retailers track revenue per square foot, we do similar analyses of our facilities,” he says.
Another key principle at Froedtert: “Provide the right care at the right place at the right time.” This strategy prompts expansion to communities so that patients have convenient access to care. “Utilization goes hand in hand with efficiency,” says Balzer. That means before the organization builds or leases new space, it looks to add evening and weekend hours at existing facilities. This can keep down costs on real estate, as well as increase convenience for patients—another key organizational goal.
New technology is impacting capital planning at the academic medical campus. A project to bring 30 operating suites up to modern standards in order to accommodate the latest surgical equipment is under design. “Thirteen operating rooms are under 500 sf,” says Balzer. “The standard today is 650 sf and up.”
The editors wish to thank the following healthcare capital planning executives for serving as experts for this report:
Rick Albert, Director of Plant Operations, MaineGeneral Medical Center
John A. Balzer, MSEM, Vice President, Facility Planning and Development, Froedtert & the Medical College of Wisconsin
Dan Conwell, AIA, NCARB, Director, Planning, Architecture and Design, Sutter Health
Bob McCoole, Senior Vice President, Facilities Resource Group, Ascension Health
Carl Scheuerman, FACHE, Director, Regulatory Affairs, Sutter Health
Paul Stein, Chief Operating Officer, MaineGeneral Medical Center
Jim Young, Director, Capital Project Management, CHE Trinity Health
Related Stories
Sustainability | Jan 9, 2023
Innovative solutions emerge to address New York’s new greenhouse gas law
New York City’s Local Law 97, an ambitious climate plan that includes fines for owners of large buildings that don’t significantly reduce carbon emissions, has spawned innovations to address the law’s provisions.
Fire and Life Safety | Jan 9, 2023
Why lithium-ion batteries pose fire safety concerns for buildings
Lithium-ion batteries have become the dominant technology in phones, laptops, scooters, electric bikes, electric vehicles, and large-scale battery energy storage facilities. Here’s what you need to know about the fire safety concerns they pose for building owners and occupants.
Market Data | Jan 6, 2023
Nonresidential construction spending rises in November 2022
Spending on nonresidential construction work in the U.S. was up 0.9% in November versus the previous month, and 11.8% versus the previous year, according to the U.S. Census Bureau.
Industry Research | Dec 28, 2022
Following a strong year, design and construction firms view 2023 cautiously
The economy and inflation are the biggest concerns for U.S. architecture, construction, and engineering firms in 2023, according to a recent survey of AEC professionals by the editors of Building Design+Construction.
Performing Arts Centers | Dec 23, 2022
Diller Scofidio + Renfro's renovation of Dallas theater to be ‘faithful reinterpretation’ of Frank Lloyd Wright design
Diller Scofidio + Renfro recently presented plans to restore the Kalita Humphreys Theater at the Dallas Theater Center (DTC) in Dallas. Originally designed by Frank Lloyd Wright, this theater is the only freestanding theater in Wright’s body of work.
University Buildings | Dec 22, 2022
Loyola Marymount University completes a new home for its acclaimed School of Film and Television
California’s Loyola Marymount University (LMU) has completed two new buildings for arts and media education at its Westchester campus. Designed by Skidmore, Owings & Merrill (SOM), the Howard B. Fitzpatrick Pavilion is the new home of the undergraduate School of Film and Television, which is consistently ranked among the nation’s top 10 film schools. Also designed by SOM, the open-air Drollinger Family Stage is an outdoor lecture and performance space.
Adaptive Reuse | Dec 21, 2022
University of Pittsburgh reinvents century-old Model-T building as a life sciences research facility
After opening earlier this year, The Assembly recently achieved LEED Gold certification, aligning with the school’s and community’s larger sustainability efforts.
Multifamily Housing | Dec 20, 2022
Brooks + Scarpa-designed apartment provides affordable housing to young people aging out of support facilities
In Venice, Calif., the recently completed Rose Apartments provides affordable housing to young people who age out of youth facilities and often end up living on the street. Designed by Brooks + Scarpa, the four-story, 35-unit mixed-use apartment building will house transitional aged youths.
Coatings | Dec 20, 2022
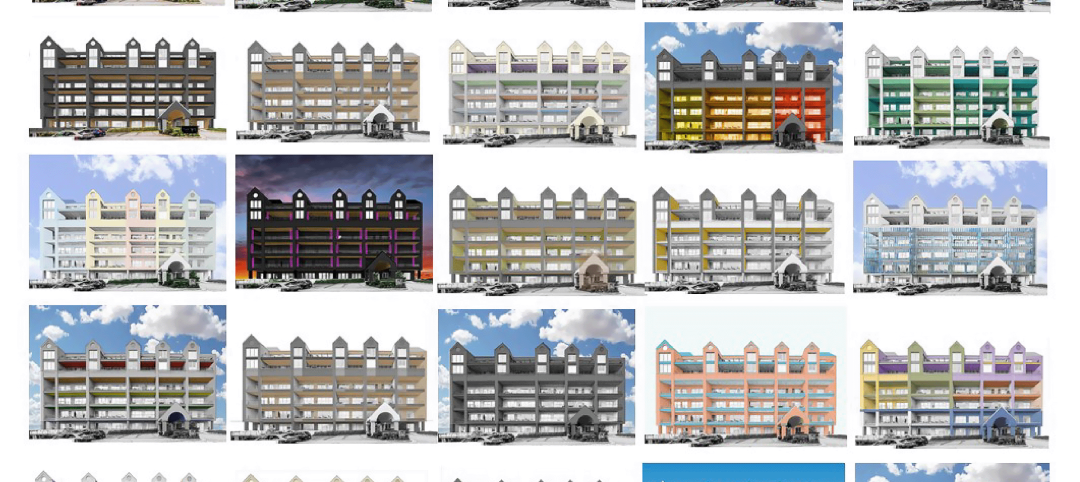
The Pier Condominiums — What's old is new again!
When word was out that the condominium association was planning to carry out a refresh of the Pier Condominiums on Fort Norfolk, Hanbury jumped at the chance to remake what had become a tired, faded project.
Cladding and Facade Systems | Dec 20, 2022
Acoustic design considerations at the building envelope
Acentech's Ben Markham identifies the primary concerns with acoustic performance at the building envelope and offers proven solutions for mitigating acoustic issues.