With increasing demand to reduce the cost of operation, healthcare leadership is challenging their facility engineers to increase efficiency of the buildings they manage. Healthcare owners are struggling with the need to improve the bottom line with limited capital to spend on projects even with the best rate of return. The return on investment is typically much more attractive and more visible when related to the addition of clinical services as opposed to an investment in infrastructure.
However, studies have shown that when looking at the total lifecycle cost for a healthcare facility, 87 percent of the total cost is spent once healthcare owners start operating the new facility, with almost half of that cost allocated to utilities. The right approach during the planning, design and construction of a new facility can yield a positive return on investment and lower the overall cost basis for ongoing operations.
Form Follows Function
As with any new endeavor, the challenge is to have the right strategy, process and tools and then utilize the latest technology and systems to achieve maximum efficiencies. To have effective facility management, healthcare owners must invest the time to determine how to best manage and operate their facilities. With little to no additional premium in construction, systems can be incorporated into the design of a new facility project that will meet the technical capabilities of existing staff. If additional capabilities are required to meet the new systems goals, identification should be made early to allow for proper training and implementation. Additionally, a clear understanding of the volume of operations that will be outsourced will have an impact on the type of systems that will be built. In architecture, the phrase form follows function is often used. This is highly applicable to systems development as well.
Vital to success is the creation of an infrastructure plan concept. Healthcare leadership can implement this critical step in conjunction with a facility master plan. Development of the plan should begin with a review of the following:
1. Hospital leadership’s vision as it relates to focus on “non-core” services
2. Existing staff capabilities and their readiness to maintain complex systems
3. Number of full-time employees and level of staffing
4. Cost of purchasing utilities
5. Level of outsourcing as it relates to preventive maintenance and service contracts
6. Availability of skilled workforce in the market
7. Hospital’s financial strength to absorb the skilled workforce
8. Structure - single entity or part of a larger system
9. Level of sharing workforce within the hospital system
10. Centralization options within the system
11. Standardization within the hospital system (inventory and purchasing strength)
12. Method of acquiring and purchasing service contracts
13. Number and location of off-site facilities — owned verses leased
14. Energy baseline for the existing facilities
15. Level of modernization and implementation of the right technology
Reviewing, evaluating and developing strategies to close the gaps in the data discussed above forms the basis of an infrastructure plan concept.
As more hospitals are becoming part of larger systems, opportunities exist to capitalize on the economies of scale. Healthcare leaders are experiencing increased responsibility for managing multiple locations, many of which are off-site. Centralizing operations, negotiating and bundling service contracts for the entire system, implementing the right technology to network all facilities, eliminating duplications with staffing and “right staffing” are all areas in which savings can be realized.
To reduce the utility costs, many are negotiating new purchasing agreements utilizing large purchasing groups. However, the demand side of business requires additional investments to also reduce the cost of consumption. With limited resources and capital available, creative measures that require minimal investment need to be implemented to reduce the demand.
Streamlining Operations
● Utilize the latest in technology to reduce the energy cost and improve staffing efficiencies by standardizations, centralizations and sharing resources. Examples of these initiatives include ensuring all systems are commissioned during any new installation and identifying the utility baseline and Energy Star rating and comparing to industry standards.
● Conduct retro-commissioning of the existing systems at locations where there are opportunities to reduce cost. Identify any deficiencies and shortcomings. Opportunities to reduce cost may be as important as reducing liabilities by ensuring systems are operating optimally, per code and can provide patient comfort and safety.
● Ensure that existing service contractors and staff make necessary corrections to systems. Typically most are processed through the existing maintenance work order system. Experience has shown that the majority of such corrections require minimum investments.
● Provide continuous commissioning via a remote monitoring program to identify “bad habits” and modify the way the systems are maintained and operated in order to reduce costs.
● Make adjustments and correct bad habits to optimize performance and reduce energy consumption. These adjustments typically require limited expenditure.
● Utilize technology to share information between facilities and improve staff efficiencies. Examples are dispatching more trained staff from a central location or reduce the staffing on remote locations by reporting alarms to a central location.
It should be noted that the latter steps cannot be implemented unless more advanced energy management and remote monitoring capabilities are in place. The implementation of such technologies will be cost prohibitive unless implemented while a major capital project takes place. This re-emphasizes the importance of planning and having the right process in place during project launch and delivery.
Conclusion
Ultimately, the direction taken to create a more efficient building and systems must be strategic. If an organization is planning a capital expansion there will be more tools and options with which to work. However, if there is no immediate capital plan to be the catalyst for this effort, then retrofit tactics could be employed. By following a structured plan through the capital delivery process a more efficient building can be achieved. The simplistic formula begins with the right concept that is an extension of the strategic vision.
Related Stories
| Oct 13, 2010
Prefab Trailblazer
The $137 million, 12-story, 500,000-sf Miami Valley Hospital cardiac center, Dayton, Ohio, is the first major hospital project in the U.S. to have made extensive use of prefabricated components in its design and construction.
| Oct 13, 2010
Hospital tower gets modern makeover
The Wellmont Holston Valley Medical Center in Kingsport, Tenn., expanded its D unit, a project that includes a 243,443-sf addition with a 12-room operating suite, a 36-bed intensive care unit, and an enlarged emergency department.
| Oct 13, 2010
Hospital and clinic join for better patient care
Designed by HGA Architects and Engineers, the two-story Owatonna (Minn.) Hospital, owned by Allina Hospitals and Clinics, connects to a newly expanded clinic owned by Mayo Health System to create a single facility for inpatient and outpatient care.
| Oct 13, 2010
Maryland replacement hospital expands care, changes name
The new $120 million Meritus Regional Medical Center in Hagerstown, Md., has 267 beds, 17 operating rooms with high-resolution video screens, a special care level II nursery, and an emergency room with 53 treatment rooms, two trauma rooms, and two cardiac rooms.
| Oct 13, 2010
Cancer hospital plans fifth treatment center
Construction is set to start in December on the new Cancer Treatment Centers of America’s $55 million hospital in Newnan, Ga. The 225,000-sf facility will have 25 universal inpatient beds, two linear accelerator vaults, an HDR/Brachy therapy vault, and a radiology and imaging unit.
| Oct 13, 2010
New health center to focus on education and awareness
Construction is getting pumped up at the new Anschutz Health and Wellness Center at the University of Colorado, Denver. The four-story, 94,000-sf building will focus on healthy lifestyles and disease prevention.
| Oct 13, 2010
Community center under way in NYC seeks LEED Platinum
A curving, 550-foot-long glass arcade dubbed the “Wall of Light” is the standout architectural and sustainable feature of the Battery Park City Community Center, a 60,000-sf complex located in a two-tower residential Lower Manhattan complex. Hanrahan Meyers Architects designed the glass arcade to act as a passive energy system, bringing natural light into all interior spaces.
| Oct 12, 2010
Holton Career and Resource Center, Durham, N.C.
27th Annual Reconstruction Awards—Special Recognition. Early in the current decade, violence within the community of Northeast Central Durham, N.C., escalated to the point where school safety officers at Holton Junior High School feared for their own safety. The school eventually closed and the property sat vacant for five years.
| Sep 13, 2010
Palos Community Hospital plans upgrades, expansion
A laboratory, pharmacy, critical care unit, perioperative services, and 192 new patient beds are part of Palos (Ill.) Community Hospital's 617,500-sf expansion and renovation.
| Sep 13, 2010
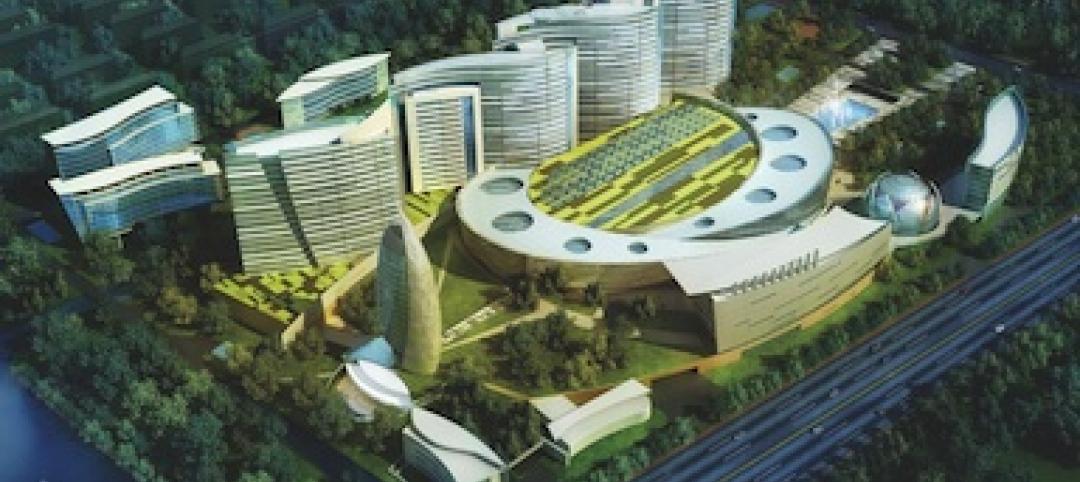
China's largest single-phase hospital planned for Shanghai
RTKL's Los Angles office is designing the Shanghai Changzheng New Pudong Hospital, which will be the largest new hospital built in China in a single phase.