With more than $38 billion spent on healthcare construction this year in the U.S alone, there is a tremendous opportunity for capital projects to incorporate efficiency, safety, and patient-centered care well before the first shovel strikes the ground.
Healthcare clients, under extreme pressure to reduce costs, desperately needed a new paradigm. In response, Lean Led Design practices have emerged. This new way of thinking requires healthcare organizations to evaluate workflow and processes, identify opportunities to remove non-value waste, and drive bottom-line results prior to major capital spending.
Nationally, our healthcare clients and project teams are embracing Lean principles, which were originally developed for manufacturing. In addition, they are adopting Lean Led Design practices and integrating continuous process improvement teams to help reduce costs, address staffing shortages, and, most importantly, increase the organization’s ability to see more patients.
BEGINNING A LEAN JOURNEY
The requisite for every project team engaged in a Lean journey is to create a safe environment where high-quality care can be delivered efficiently to achieve the best possible outcomes. Project teams must engage frontline staff to help identify operational waste, consider alternative ways to do the work, and develop design recommendations and guardrails for the capital project.
Before the first deep dive into finding non-value waste or discussing different ways to do the same task, healthcare owners and project teams must understand the construction timeline, budget constraints, and other key project guardrails to set the project parameters and milestones for the team. With end dates in mind, the project team can define how Lean should be integrated into the facility planning and design process and determine if a Lean Led Design approach makes the most sense.
Not all projects afford teams a lengthy Lean journey. The challenge for most capital projects is speed to market. The time it takes to design, construct, and occupy varies for every project and must be carefully considered when deciding on whether to integrate process improvement efforts into the design schedule. The window of opportunity to contemplate process changes or new models for an improved future state in the new space must be defined and may not afford a traditional design approach.
LEAN LED DESIGN
For projects that are more time-critical, a Lean Lead Design approach offers healthcare owners an abbreviated design process. All key stakeholders and leadership are brought together in a series of collaborative design events that begin with training staff on how to critically assess where and how the care is being delivered and how to quickly identify process waste that doesn’t bring value to the patient or the organization.
Design teams work closely with staff to understand the role the environment plays in implementing many of the suggested operational improvements and begin to develop conceptual design solutions, as well as programmatic and functional space requirements.
When considering new ideas, Lean principles guide the entire project team to always keep patients at the front and center of the process and never lose sight of what is best for the patient.
Lean Led Design is a collaborative approach and affords healthcare organizations to quickly identify many process improvements that may not have surfaced in a traditional department user group meeting.
The 3P Lean Event, which stands for product (patient care), process, and preparation, is based on the Toyota production process and engages end users closest to the work along with the entire project planning team. The project's architects, engineers, construction management team, and hospital leadership join the clinical teams and support staff in a vetting process of ideas. Many ideas are weeded out due to lack of support by others involved, limited resources, cost, and implementation issues.
The approach pushes teams to gain organizational support for process changes and collectively recommend those that would yield the greatest cost savings or best outcomes. This doesn’t always happen in traditional departmental level user group meetings where clinical teams mostly focus on the process that occurs within their immediate departmental boundaries and rarely have the opportunity to discuss the entire process with leadership, support staff, and other departmental teams.
By understanding the baseline and identifying reasonable future state targets that are measurable, healthcare owners and project teams can assess if the new approaches developed during 3P Lean Events truly improve quality and performance and reduce cost. 3P Lean Events fully integrate process design, functional space programming, and healthcare planning into a series of 2D and 3D modeling exercises that enables stakeholders to work out design details at a room-by-room level while keeping a broader focus on departmental adjacencies, intra-departmental connections, and systemwide opportunities and savings.
During many events, several process improvements are identified that could be implemented immediately into existing space rather than waiting for the new project to implement. Organizations are afforded more time to perfect the new process prior to moving into a new space.
LEAN PRINCIPLES
The Lean principles that guide project teams during Lean events include:
• Value: Only the healthcare consumer can determine value. Unnecessary tests or lengthy wait times do not add value to the patient experience, and these activities represent non-value added waste. Neither a physician nor a CEO can determine value, but they can drive value when focused on the needs of the community and healthcare consumer. There is also a constant balancing act in healthcare process design between the optimal patient experience and an optimal work environment. During Lean events, it is important to engage focus groups or have someone consistently be the voice of the patient to help drive balance between workplace preferences that override patient experience.
• Value Stream: The value stream describes the sequence of activities for a healthcare service or process that produces value. For example, an admissions process where a patient provides personal information once and caregivers have the medical history readily available from a pre-admissions process streamlines the time it takes the patient to arrive, receive a barcoded wristband, and receive healthcare services.
• Flow: Optimal flow is created when non-value added activities are removed from the value stream.
• Pull: The “pull” means the healthcare system only provides a service or product when the consumer signals the need. A great example of pull is in healthcare organizations that implemented par levels systems, like Omnicells or Pyxis machines, to track medications and materials per consumer. For environmental services, pull means the service of collecting soiled linens. Rather than collect linens a few times a day, which is a great example of batching work, a linen chute could be installed so soiled linens move immediately off the inpatient unit and are available for processing.
• Perfection: This principle is to always strive for perfection in all value streams and to remember: perfection should always be considered from the perspective of the healthcare consumer.
PROCESS WASTE
In healthcare facilities, there are eight areas of process waste typically discussed in a 3P Lean Event:
• Overproduction
• Waiting
• Inefficient conveyance
• Confusion
• Rework
• Excess inventory
• Unnecessary motion, such as overly long walking distances for nursing staff or excessive patient transport
• Correction, or steps undertaken to remedy situations caused by wasteful practices.
Understanding the root cause of the waste will help teams better address alternative options and assess if the countermeasure will rid the waste and non-value add from the process.
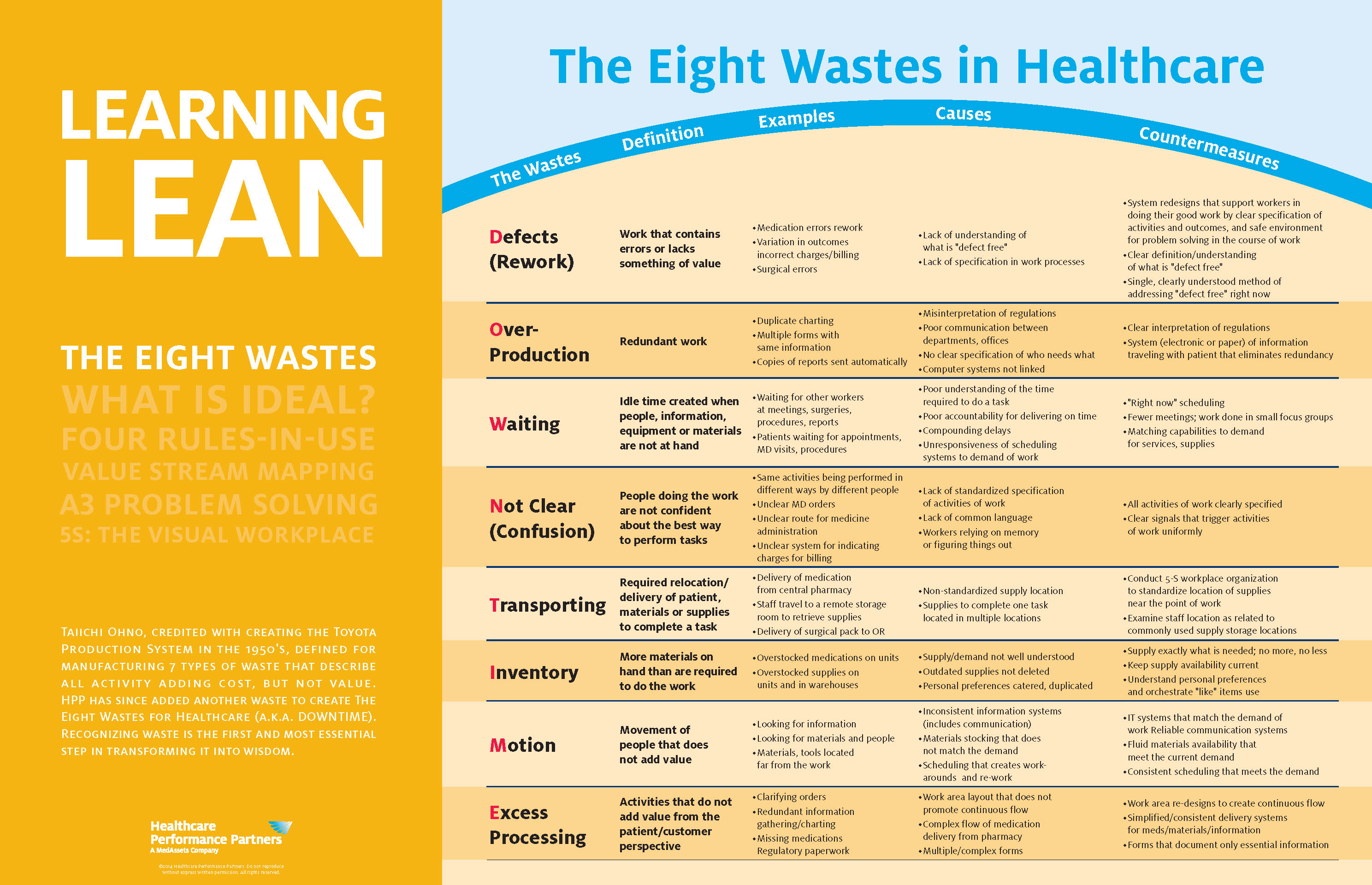
Source: Healthcare Performance Partners. CLICK IMAGE TO ENLARGE
CONCLUSION
Are you about to embark on a Lean journey for your next major capital project? Healthcare owners should understand the initial investment of staff resources required to conduct Lean Led Design events and how important it is that leadership remains engaged in the process.
Continuous process improvement teams and leadership must be willing to embrace change and do what it takes to implement it. Consider outside resources to help train staff in Lean Led Design, facilitate 3P Lean Led Design events, and assist in transforming organizational culture towards a future state that consistently seeks to improve operations, improve quality, be more patient centered, and reduce healthcare costs.
Related Stories
Adaptive Reuse | Oct 22, 2024
Adaptive reuse project transforms 1840s-era mill building into rental housing
A recently opened multifamily property in Lawrence, Mass., is an adaptive reuse of an 1840s-era mill building. Stone Mill Lofts is one of the first all-electric mixed-income multifamily properties in Massachusetts. The all-electric building meets ambitious modern energy codes and stringent National Park Service historic preservation guidelines.
MFPRO+ News | Oct 22, 2024
Project financing tempers robust demand for multifamily housing
AEC Giants with multifamily practices report that the sector has been struggling over the past year, despite the high demand for housing, especially affordable products.
Performing Arts Centers | Oct 21, 2024
The New Jersey Performing Arts Center breaks ground on $336 million redevelopment of its 12-acre campus
In Newark, N.J., the New Jersey Performing Arts Center (NJPAC) has broken grown on the three-year, $336 million redevelopment of its 12-acre campus. The project will provide downtown Newark 350 mixed-income residential units, along with shops, restaurants, outdoor gathering spaces, and an education and community center with professional rehearsal spaces.
Office Buildings | Oct 21, 2024
3 surprises impacting the return to the office
This blog series exploring Gensler's Workplace Survey shows the top three surprises uncovered in the return to the office.
Healthcare Facilities | Oct 18, 2024
7 design lessons for future-proofing academic medical centers
HOK’s Paul Strohm and Scott Rawlings and Indiana University Health’s Jim Mladucky share strategies for planning and designing academic medical centers that remain impactful for generations to come.
Sports and Recreational Facilities | Oct 17, 2024
In the NIL era, colleges and universities are stepping up their sports facilities game
NIL policies have raised expectations among student-athletes about the quality of sports training and performing facilities, in ways that present new opportunities for AEC firms.
Codes and Standards | Oct 17, 2024
Austin, Texas, adopts AI-driven building permit software
After a successful pilot program, Austin has adopted AI-driven building permit software to speed up the building permitting process.
Resiliency | Oct 17, 2024
U.S. is reducing floodplain development in most areas
The perception that the U.S. has not been able to curb development in flood-prone areas is mostly inaccurate, according to new research from climate adaptation experts. A national survey of floodplain development between 2001 and 2019 found that fewer structures were built in floodplains than might be expected if cities were building at random.
Seismic Design | Oct 17, 2024
Calif. governor signs limited extension to hospital seismic retrofit mandate
Some California hospitals will have three additional years to comply with the state’s seismic retrofit mandate, after Gov. Gavin Newsom signed a bill extending the 2030 deadline.
MFPRO+ News | Oct 16, 2024
One-third of young adults say hurricanes like Helene and Milton will impact where they choose to live
Nearly one-third of U.S. residents between 18 and 34 years old say they are reconsidering where they want to move after seeing the damage wrought by Hurricane Helene, according to a Redfin report. About 15% of those over age 35 echoed their younger cohort’s sentiment.

















