A recent poll of healthcare providers found that 85% agree that most patients will not require an in-person physician evaluation by 2021. Virtual doctor visits will be common, smartphones and wearable sensors will be used widely to record a patient’s health information, and patients will have greater access to self-serving their health needs via technology equipped unmanned kiosks.
These are some of the predictions from the Mortenson Leadership Series Healthcare Study, the construction firm’s fourth in the last six years. The study is based on a poll of more than 900 healthcare professionals, facilities leaders, and architects who support them, conducted during last year’s ASHE Planning, Design, and Construction Summit.
While most of the study’s findings weren’t surprising, they confirm trends about Millennials’ healthcare expectations, how and where healthcare institutions will be investing, the role of technology in healthcare, and what roadblocks might lie ahead for project management.

Millennials' preferences for how they receive healthcare are having a major impact on how health systems are investing. Image: Mortenson
One thing is certain: patients are taking more ownership of their health. Eighty-three percent of the healthcare providers polled observe that patients are far more willing these days to shop for lower-cost care options. By 2021, 85% predict that providers will screen patients first to guide them to the appropriate treatment. And that won’t necessarily be toward a medical office or clinic.
One of the biggest disparities between the 2018 and 2015 surveys was the responses to the question about how common virtual doctors would be in three years’ time. Last year, 88% responded to this question affirmatively, compared to 63% in 2015. And 85% in the 2018 surveyed participants thought that most patients don’t require an in-person physician evaluation, versus 49% in 2015.
As one 2018 respondent noted, “Millennials expect immediate access. This access will drive how we design facilities as well as garner a new age of telehealth.” Two-fifths of healthcare providers and architects mentioned that virtual telemedicine and self-service treatments would be typical delivery care within the next decade, with much less reliance on physical structures to deliver goods and services.
Healthcare facilities managers say their institutions must become leaner to grapple with insufficient project resources. Many see opportunities in reducing waste and energy consumption. Image: Mortenson
More than two-fifths (44%) of architects polled also said that Millennials’ expectations about the need for more integration and utilization of technology is impacting healthcare and its facilities, followed by 22% who cited the demand for convenience and virtual care. “Less acute, more ambulatory. Less invasive procedures. More virtual … diagnosis and treatments,” stated one respondent.
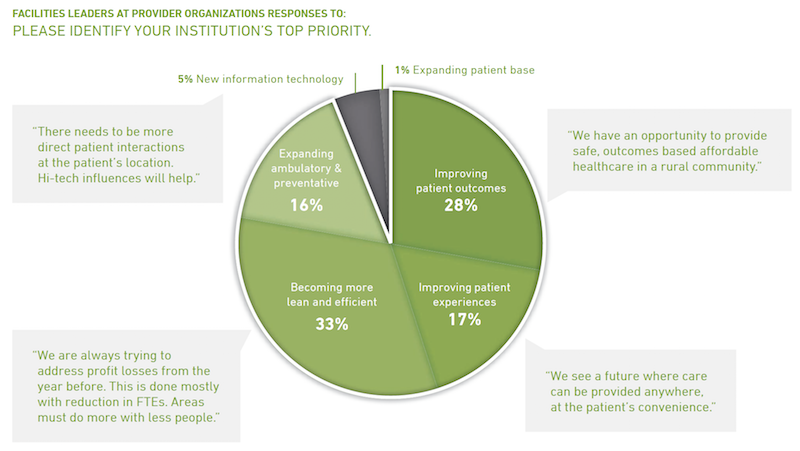
Two thirds of facilities leaders polled said that their institutions would invest more over the next two to three years. But 35% added that their biggest challenge continues to be insufficient money and resources (including receiving adequate payments for services rendered), followed by “growing pains” (18%) and project delivery (17%).
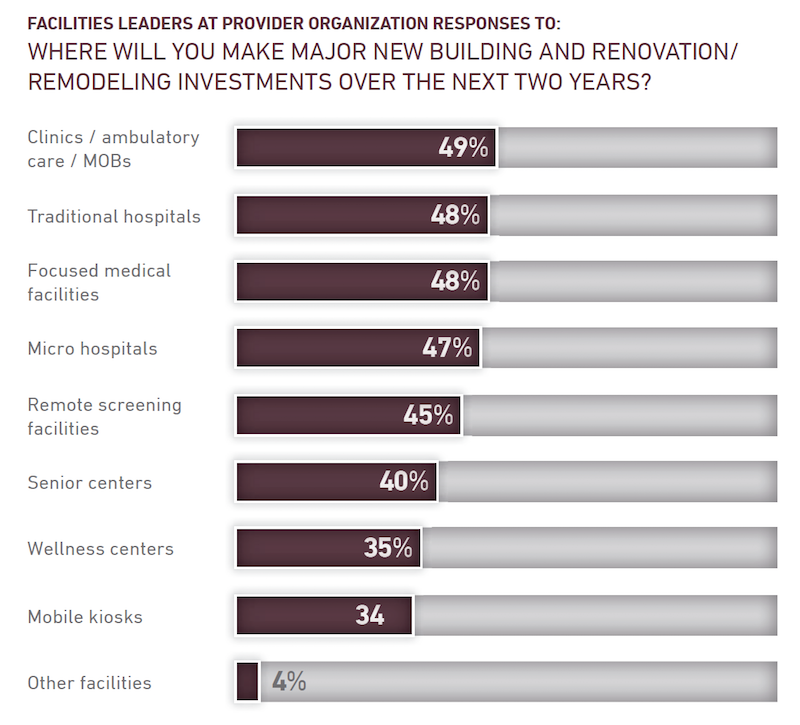
Nearly half of facilities leaders polled say their healthcare systems continue to invest in clinics, ambulatory care centers, and medical offices. Image: Mortenson
Nearly all of the facilities leaders see significant opportunities to eliminate waste and reduce energy use.
Despite all of speculation about virtual care expressed in the study, 49% of facilities leaders said their institutions would be making major investments in clinics, ambulatory care, and MOBs, followed by traditional hospitals and focused medical facilities (48% each), microhospitals (47%), and remote screening facilities (45%).
The respondents were evenly split about how much their institutions might spend over the next two years, with 33% each projecting moderate, substantial, or flat growth.
The study includes a section about the Affordable Care Act. Fewer respondents in 2018 than in 2015 thought the legislation had done enough to address the country’s long-term healthcare needs. And between 94% and 97% of those polled last year said that the Act still needed “significant changes or revisions,” had created uncertainty for their institutions, and had challenged their organization’s near-term financial condition.
Related Stories
| Aug 11, 2010
Stimulus funding helps get NOAA project off the ground
The award-winning design for the National Oceanic and Atmospheric Administration’s new Southwest Fisheries Science Center replacement laboratory saw its first sign of movement last month with a groundbreaking ceremony held in La Jolla, Calif. The $102 million project is funded primarily by the American Recovery and Reinvestment Act.
| Aug 11, 2010
National Intrepid Center tops out at Walter Reed
SmithGroup, Turner Construction, and the Intrepid Fallen Heroes Fund (IFHF), a nonprofit organization supporting the men and women of the United States Armed Forces and their families, celebrated the overall structural completion of the National Intrepid Center of Excellence (NICoE), an advanced facility dedicated to research, diagnosis, and treatment of military personnel and veterans sufferin...
| Aug 11, 2010
Alabama hospital gets a four-story addition
Birmingham, Ala.-based Hoar Construction has completed the North Tower addition at Thomas Hospital in Fairhope, Ala. The four-story, 123,000-sf addition accommodates an ER on the first floor, 32 private patient rooms and nursing support on the second and third floors, and room for 32 planned patient rooms on the top floor.
| Aug 11, 2010
America's Greenest Hospital
Hospitals are energy gluttons. With 24/7/365 operating schedules and stringent requirements for air quality in ORs and other clinical areas, an acute-care hospital will gobble up about twice the energy per square foot of, say, a commercial office building. It is an achievement worth noting, therefore, when a major hospital achieves LEED Platinum status, especially when that hospital attains 14 ...
| Aug 11, 2010
Hospital Additions + Renovations: 14 Lessons from Expert Building Teams
Two additions to a community hospital in Ohio that will double its square footage. A 12-story addition on top of an existing 12-story tower at Houston's M.D. Anderson Cancer Center. A $54 million renovation and addition at the University of Virginia Medical Center. A 67-bed, $70 million addition/renovation to a community hospital that is only five years old.
| Aug 11, 2010
Research Facility Breaks the Mold
In the market for state-of-the-art biomedical research space in Boston's Longwood Medical Area? Good news: there are still two floors available in the Center for Life Science | Boston, a multi-tenant, speculative high-rise research building designed by Tsoi/Kobus & Associates, Boston, and developed by Lyme Properties, Hanover, N.
| Aug 11, 2010
3 Hospitals, 3 Building Teams, 1 Mission: Optimum Sustainability
It's big news in any city when a new billion-dollar hospital is announced. Imagine what it must be like to have not one, not two, but three such blockbusters in the works, each of them tracking LEED-NC Gold certification from the U.S. Green Building Council. That's the case in San Francisco, where three new billion-dollar-plus healthcare facilities are in various stages of design and constructi...
| Aug 11, 2010
Holyoke Health Center
The team behind the new Holyoke (Mass.) Health Center was aiming for more than the renovation of a single building—they were hoping to revive an entire community. Holyoke's central business district was built in the 19th century as part of a planned industrial town, but over the years it had fallen into disrepair.
| Aug 11, 2010
Right-Sizing Healthcare
Over the past 30 years or so, the healthcare industry has quietly super-sized its healthcare facilities. Since 1980, ORs have bulked up in size by 53%, acute-care patient rooms by 77%. The slow creep went unlabeled until recently, when consultant H. Scot Latimer applied the super-sizing moniker to hospitals, inpatient rooms, operating rooms, and other treatment and administrative spaces.
| Aug 11, 2010
Great Solutions: Healthcare
11. Operating Room-Integrated MRI will Help Neurosurgeons Get it Right the First Time A major limitation of traditional brain cancer surgery is the lack of scanning capability in the operating room. Neurosurgeons do their best to visually identify and remove the cancerous tissue, but only an MRI scan will confirm if the operation was a complete success or not.







