Michael Sheerin, PE, CEO of TLC Engineering Solutions, chairs the ASHRAE Standard 170 committee, which covers the ventilation of healthcare facilities. A 25-plus-year veteran of designing mechanical systems for healthcare, Sheerin and colleagues at ASHRAE, ASHE, and TLC have created a PDF document (updated almost daily) to advise design, engineering, and construction professionals as to the nuances of ventilation for facilities where COVID-19 patients are being treated.
NOTE: The guidance referenced here is based on input from ASHE, the ASHRAE Technical Committee for Healthcare, and the ASHRAE/ASHE Standard 170 Committee. The guidance represents the personal opinions of TLC Senior Healthcare Engineering staff. ASHRAE and ASHE are not responsible for the use or application of this information. For further information, contact: Michael.sheerin@tlc-eng.com.
 Use of hospital auditorium for post-acute care.
Use of hospital auditorium for post-acute care.
Here are key highlights of the TLC document.
SETTING UP AND IMPLEMENTING THE ACTION PLAN
Health facility operators should first verify the performance of any existing airborne infectious isolation (AII) rooms in their facilities, as well as the performance of the emergency department HVAC system. All HEPA units should be secured, and plans for a patient surge and temporary patient segregation should be readied for deployment.
The primary function and expertise of healthcare engineers in preparing healthcare facilities for COVID-19 is advising on HVAC systems, configurations, and modifications to support the safe segregation of suspected and confirmed patients within controlled-air environments, whether true isolation or modified alternative arrangements.
Basic advice: Keep it simple. In terms of resource management, recognize that you have limited time, so focus your efforts. Don’t waste time or dollars if you don’t have clear goals and a plan. Work with clinicians in the facility to establish minimum standards, define key spatial areas and designated rooms or suites for airborne infectious isolation. Maintain all life safety precautions. Draw a floor plan or map, and make sure everyone involved understands it.
THE BASICS OF PASSIVE ISOLATION
As prescribed in CDC Guidance, the most basic approach is “one patient per room, close the door.” Healthcare engineers should implement related CDC safety protocols and work with clinicians to anticipate patient load and establish a layered approach as needed.
In implementing a layered approach, hospital facilities and their engineering consultants should be aware of the various clinical modes:
- “Normal Mode” - Follow CDC guidelines. The clinical plan may limit airborne infection isolation rooms to patients receiving aerosol-generating procedures.
- “Small-scale Surge Capacity Mode” – The project team may be asked to create additional dedicated AII or temporary patient observation/segregation rooms with HEPA and negative pressure.
- “Large-scale Surge Capacity Mode” – The team may be asked to establish dedicated wards or suites and establish protocols with clinical and environmental action plans.
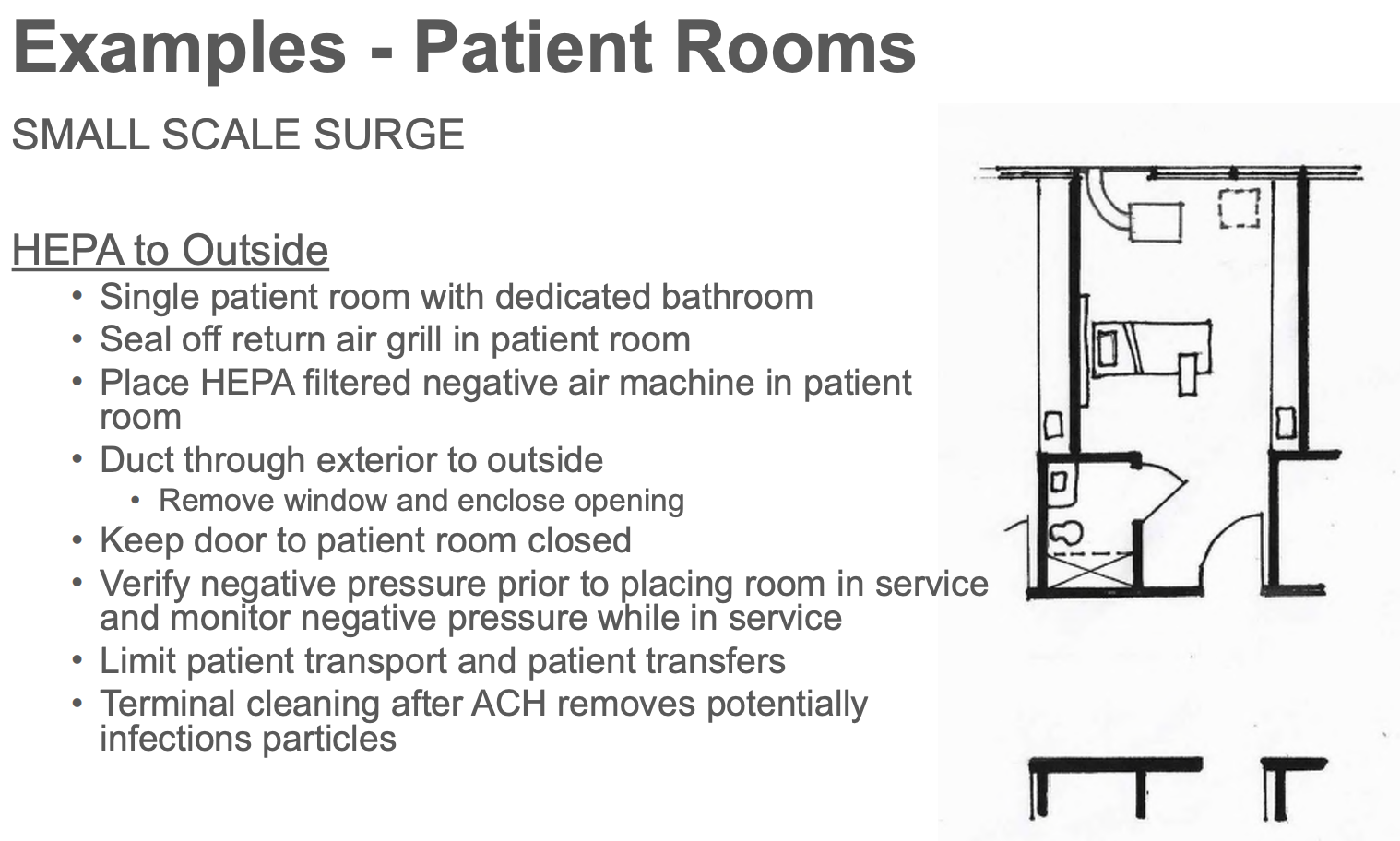 Floor plan for a small-surge COVID-19 patient room with optimal ventilation.
Floor plan for a small-surge COVID-19 patient room with optimal ventilation.
The report recommends informing clinicians that temporary patient observation or segregation areas are not true AII rooms.
The document also provides guidance on patient rooms and ICUs and ORs (for use with COVID patients and as alternative ICU space).
The document also provides information on personal protection equipment (PPE) and ventilators.
CREATING ALTERNATE CARE SITES
In developing alternate care sites, project teams should be clear about the clinical goals, as they will dictate the infrastructure needed. Are the alternate case sites to be used to provide care to COVID-suspected patients or non-COVID patients? At what acuity level? Don’t forget to consider liability issues if diverging from FGI or State Guidelines.
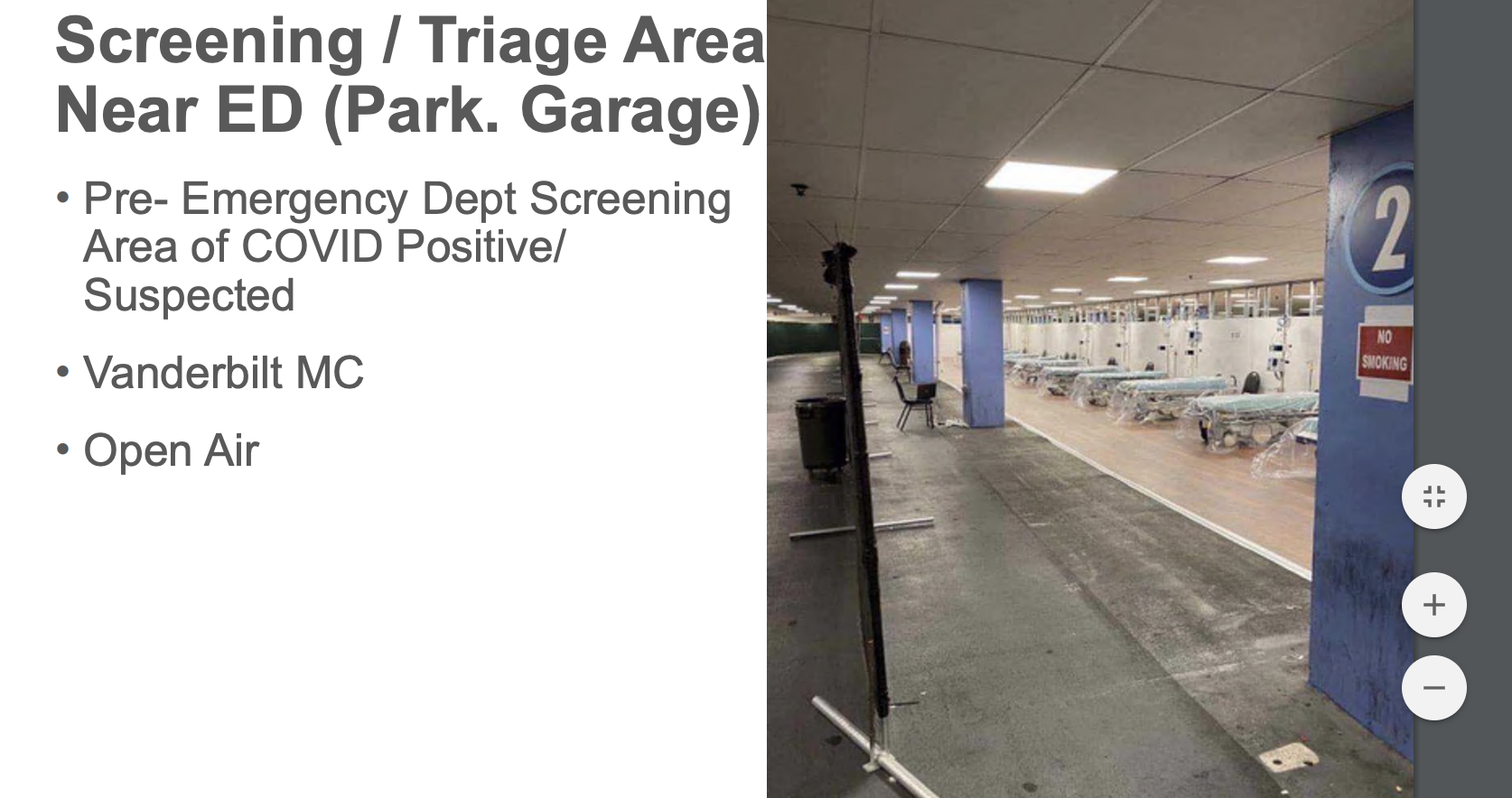 Triage area near emergency department in parking garage at Vanderbilt Medical Center, Nashville.
Triage area near emergency department in parking garage at Vanderbilt Medical Center, Nashville.
ASHE Note: During emergencies, it is important that activities be coordinated through the organization’s incident command system. Activities outside of an organization’s command structure should be coordinated with the local, county, and state incident command systems. This enables effective and efficient incident management within common organizational structures. See ASHE Resources.
Additional items to plan for and address in creating alternate care sites include the adequacy of skilled care providers and support staff; supplies: PPE, beds, equipment, and infrastructure, including HVAC, power, Wi-fi; space considerations; and site evaluation and proximity to the hospital and areas of demand.
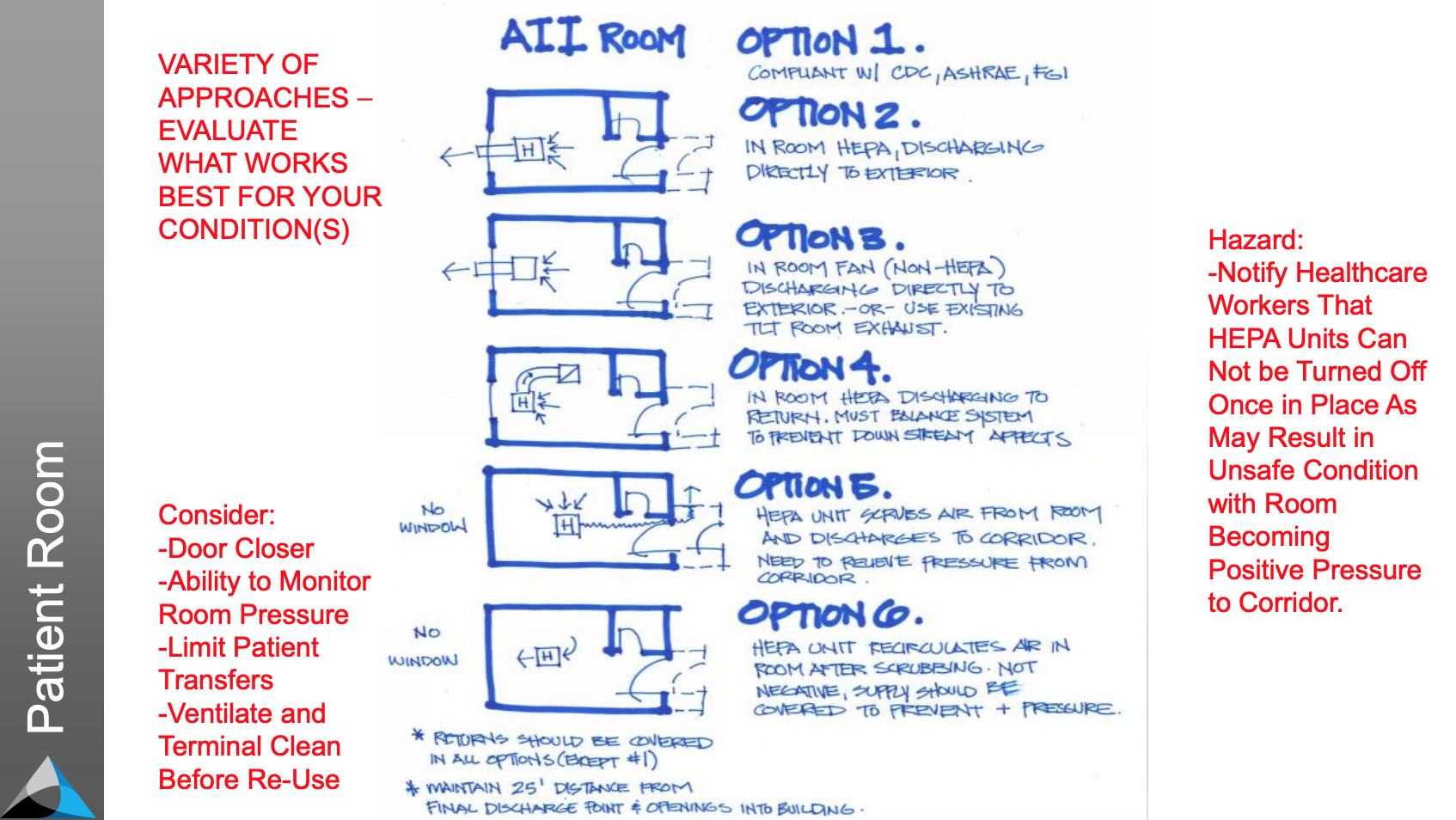 Design options for AII airborne infection control room for COVID-19 patients.
Design options for AII airborne infection control room for COVID-19 patients.
Do not ignore access to toilets and handwashing. This can be a problem at large-scale facilities like convention centers, such as the Javits Center in New York.
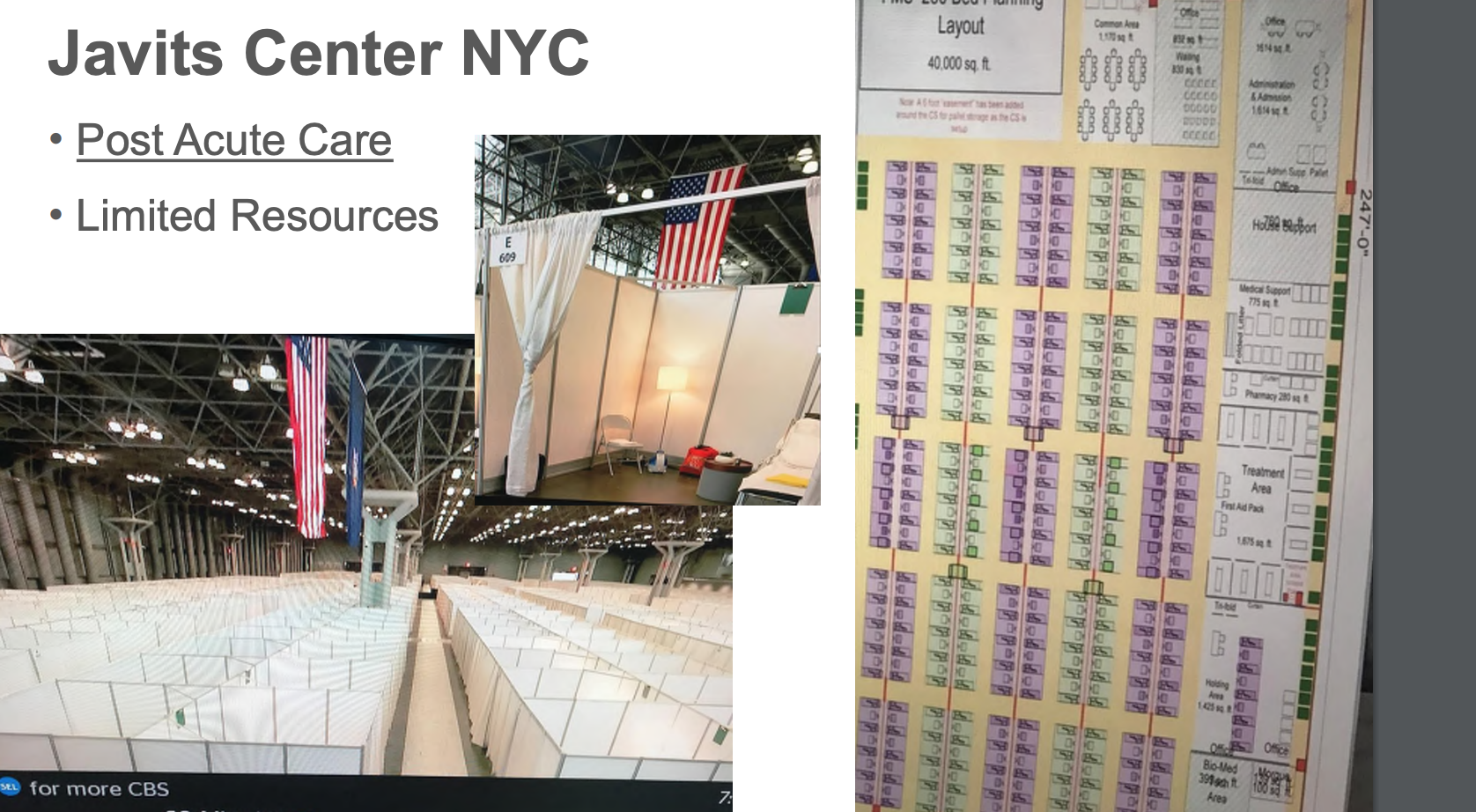
Javits Center, New York - post-acute care configuration.
CODE COMPLIANCE CONCERNS
The design team should coordinate with state and local authorities for help and take appropriate action based on circumstances and develop Interim Life Safety Measures as applicable.
Important reminder: Document the Action Plan and Alterations in Place.
Related Stories
Daylighting | Aug 18, 2022
Lisa Heschong on 'Thermal and Visual Delight in Architecture'
Lisa Heschong, FIES, discusses her books, "Thermal Delight in Architecture" and "Visual Delight in Architecture," with BD+C's Rob Cassidy.
| Aug 16, 2022
Cedars-Sinai Urgent Care Clinic’s high design for urgent care
The new Cedars-Sinai Los Feliz Urgent Care Clinic in Los Angeles plays against type, offering a stylized design to what are typically mundane, utilitarian buildings.
| Aug 15, 2022
IF you build it, will they come? The problem of staff respite in healthcare facilities
Architects and designers have long argued for the value of respite spaces in healthcare facilities.
AEC Tech | Aug 8, 2022
The technology balancing act
As our world reopens from COVID isolation, we are entering back into undefined territory – a form of hybrid existence.
| Aug 3, 2022
Designing learning environments to support the future of equitable health care
While the shortage of rural health care practitioners was a concern before the COVID-19 pandemic, the public health crisis has highlighted the importance of health equity in the United States and the desperate need for practitioners help meet the needs of patients in vulnerable rural communities.
Healthcare Facilities | Aug 1, 2022
New Phoenix VA outpatient clinic is one of the largest veteran care facilities in the U.S.
The new Phoenix 32nd Street VA Clinic, spanning roughly 275,000 sf over 15 acres, is one of the largest veteran care facilities in the U.S.
Building Team | Jul 12, 2022
10 resource reduction measures for more efficient and sustainable biopharma facilities
Resource reduction measures are solutions that can lead to lifecycle energy and cost savings for a favorable return on investment while simultaneously improving resiliency and promoting health and wellness in your facility.
Healthcare Facilities | Jun 22, 2022
Arizona State University’s Health Futures Center: A new home for medical tech innovation
In Phoenix, the Arizona State University (ASU) has constructed its Health Futures Center—expanding the school’s impact as a research institution emphasizing medical technology acceleration and innovation, entrepreneurship, and healthcare education.
Healthcare Facilities | Jun 20, 2022
Is telehealth finally mainstream?
After more than a century of development, telehealth has become a standard alternative for many types of care.
Codes and Standards | Jun 14, 2022
Hospitals’ fossil fuel use trending downward, but electricity use isn’t declining as much
The 2021 Hospital Energy and Water Benchmarking Survey by Grumman|Butkus Associates found that U.S. hospitals’ use of fossil fuels is declining since the inception of the annual survey 25 years ago, but electricity use is dipping more slowly.