Are you reeling from the recent legislation that went into effect in November mandating that any new hospital-owned physician practice more than 250 yards from the hospital’s main campus will receive reduced reimbursement from Medicare? While there are other provisions built into the Bipartisan Budget Act of 2015, Section 603 has the greatest impact on the facility design and construction industry, whether you are a provider, operator, designer or builder. I recently had the opportunity to speak with several of my colleagues to gauge their thoughts and opinions on the potential impact of this new law.
In summary, the legislation would exclude from Medicare’s Outpatient Hospital Prospective Payment System (OPPS) any new off-campus ambulatory departments of a hospital/health system, as recognized by Medicare’s provider-based standards, unless it is an emergency department. These facilities will be subjected to the lower Medicare reimbursement rates available from either the Medicare Physician Fee Schedule or the ambulatory surgery center payment system. The legislation grandfathers any such departments that have billed Medicare under the OPPS prior to the date of the legislation’s enactment, allowing them to continue to be reimbursed at the original rate. Newly constructed outpatient hospital departments that were not billing under OPPS as of November 2, 2015 will be eligible for OPPS reimbursement until December 31, 2016.
The National Law Review stated “this provision will significantly alter the willingness of hospitals to acquire off-campus clinical settings and convert them to provider-based hospital departments, as doing so would impose all the overhead of a hospital-based department, but at the lower rates available to a freestanding, often unregulated, facility.”
Will this reduced reimbursement lead to better outcomes or will quality of care be impacted? Thomas Nickels, an Executive Vice President for the American Hospital Association, stated, "This untested idea may endanger patient access to care, especially among patients who are sicker, the poor, minorities, and seniors who often receive care in hospital outpatient departments."
THE IMPACT ON AMBULATORY CARE
In the New York Tri-State region, several very large, high profile (and very expensive) ambulatory care facilities have recently been completed, or are under way, that may be impacted by the new law. The business plans for these facilities did not consider the reduced reimbursement now expected. Private ambulatory practices were already working in a reduced pricing structure but hospitals were still being reimbursed for off-campus ambulatory care as if it were hospital-based. Those private practices have learned to work within the reduced pricing structures, both in terms of planning efficiency and operation. For hospitals to succeed with this pricing structure, they must start thinking like these lean, efficient and entrepreneurial practices.

According to Cheri Clarke-Doyle of Trammell Crow Company, “Hospitals are saying they still need to go off campus to meet the needs of their population, but I wonder if that is possible with this change. With bundled payments and financial risk shifting to health systems, wouldn't less expensive settings (non-hospital based) become better alternatives in the long run?” One would think so, but with the financial impacts of this legislation unknown, healthcare providers will do what they typically do when change occurs - tread carefully.
THE IMPACT ON REAL ESTATE ACTIVITY
Chris Bodnar and Lee Asher of CBRE stated the following impact on the real estate industry, “The implementation of Section 603 is likely to positively impact the values of grandfathered off-campus facilities. Moving forward, we anticipate that these assets will become a desired asset subclass due to their rarity, and investor demand will far outweigh supply in the marketplace. Consequently, the implementation of the provision has the potential to negatively impact the allure of newly constructed facilities and those that were not actively billing under the OPPS as of November 2, 2015. Prospective purchasers will need to adjust their underwriting methodology to account for lower reimbursement rates. Additionally, we expect that developers evaluating opportunities of this nature will utilize more conservative underwriting standards in determining the opportunity costs between projects. In the near term, there is also concern that construction activity for this type of facility may slow as investors, developers, and health systems alike reassess the market and their strategies.”
HISTORY LESSON
Similar to the Patient Protection and Affordable Care Act (PPACA) which was passed several years ago, many providers have still not fully absorbed the impact or lack thereof. The PPACA challenged healthcare providers to deliver higher quality care to an expanded patient base at a significantly lower overall cost. And, while health systems have been seeking solutions to meet that challenge, this new legislation will create significant road blocks to the strategies that are currently being implemented. In an article written by Kevin Kraiss of CBRE Healthcare in 2013, he laid out the approach that systems would need to follow to successfully comply with the PPACA. Kraiss wrote, “Until very recently, prevailing expectations held that the Affordable Care Act would result in a net increase in the number of insured Americans by as many as 30 million individuals. However, the highly publicized shortcomings of government sponsored insurance enrollment portals, the relative lack of interest in enrollment among younger age cohorts and the increasing number of individuals receiving coverage cancellation notices … actually resulted in a short term decrease in the total insured population.”
“A central objective of the Affordable Care Act is to transition to a Value Based Reimbursement environment in which ‘bundled payments’ are made to coordinated teams of care providers and are based on patient outcomes rather than the number of procedures performed the traditional method of compensation. There will be little to no reimbursement for patient readmissions. This seismic shift will mandate that high quality patient outcomes are achieved consistently in the most coordinated and efficient manner possible.
“Advances in medical technology have driven a shift in procedural volume to the outpatient environment for decades. With the added imperative to provide care in the lowest cost responsible setting, this trend is expected to continue. …The hospital centric model of the past has already given way to a hub and spoke network of care in most markets, where outpatient centers provide convenient and accessible care to patients and refer volumes to affiliated inpatient facilities. The prevailing hub and spoke network will give way to a distributed model of care that is physically dispersed yet highly integrated. Electronic medical records and advances in medical information technology will allow seamless handoffs between care providers, many of whom will be geographically dispersed across the network.
“Reflecting the significant capital investment in acute care facilities and traditional medical office environments that currently resides on providers’ balance sheets, the transition of healthcare real estate portfolios to nimble, distributed networks of care will be a long term process. Given the lengthy cycle of major facility planning and development schedules, … providers initiated coordinated market and facility planning efforts immediately in order to begin their journey of transformation.”

LONG TERM TRENDS
Because providers leapt into developing these facilities, this new legislation adds additional challenges to those already looking to provide cost-effective healthcare to a broader demographic and more expansive regions. However, some healthcare providers and planning consultants were prepared for this. For an ambulatory surgery joint venture currently being structured, the reimbursement modeling assumed the reduced rates. In order to make up the difference in cost, the cost of providing care needs to decrease. How will that occur? According to Patrick Duke of CBRE Healthcare, there are three major trends occurring.
- Emphasis on managing your at-risk population: Population health initiatives will be key to controlling the frequent fliers and reducing utilization. We will see more hospitals expand their continuum of care to really focus on the 5% of the population that is responsible for 50% of the costs. For example, we are seeing many larger health systems expand their Post-Acute Care offerings and putting more focus on programs such as PACE (Programs for All-inclusive Care for the Elderly). In addition, bundled payment systems will help incentivize providers to curb utilization of higher cost care and we are in the midst of that shift. It will not be easy and will take some time to take hold. Right now, our system is based on physical encounters to justify reimbursement. Virtual encounters continue to grow in frequency but there is no real way to monetize those yet and they will account for an overwhelmingly majority of patient encounters with a system’s population in the future
- Lower costs of doing business: This includes lower cost settings from a real estate perspective in the facilities from which systems deliver care. However, code officials need to help our industry in relaxing some of the requirements for certain settings outside of the hospital so we can build at even lower costs. More effective use of physician extenders on the specialist side such as Nurse Practitioners and Physician Assistants will be necessary and again, state laws differ across the country on how much you can leverage these individuals. Another area is supplies. The supply costs in a hospital setting and the benchmarks for what you see at an off-campus ambulatory surgery center, for example, are vastly different. Hospitals pay a significantly higher rate.
- Costs shifting: Healthcare costs under the PPACA have shifted more toward individuals in the form of higher deductible plans. There are several think tanks, including Price Waterhouse Coopers that believe consumers may be deferring care at a higher rate to save money. Deferred utilization can be a good thing, but not if patients are deferring care that could potentially provide early detection of chronic diseases. If this is the case, it will lead to higher costs of care over the patient’s life. This would be counter intuitive to the goals of the PPACA.

SENIOR CARE FACILITIES
In regard to the senior care mentioned above, just how does this new legislation affect senior care facilities, particularly those that are part of a health system’s continuum of care? The vast majority of these facilities are not hospital-campus-based. Does that mean that any medical care provided will be reimbursed at a different rate if it is not standard skilled nursing care? What about on-site rehabilitation? This must be investigated further. As baby-boomers age and live longer, the demand for these facilities will continue to grow. Today, there are 75,000 Americans who are 100 years old, but by 2040 it is projected that number will swell to half a million.
WHAT CAN WE DO
Notwithstanding the politics that Duke refers to (which are the main driver), what can facilities managers and the design and construction industry do? Aside from investing in existing grandfathered facilities, following are several suggestions that expand on the thoughts in trend #2:
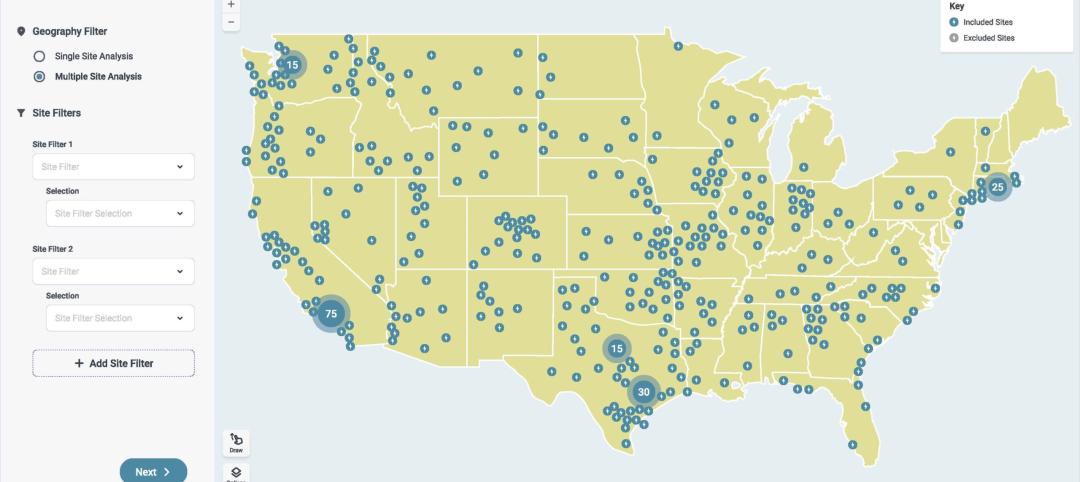
- Be smart about the markets you are servicing. Use portfolio analytics of market data and demographics to drive better decisions on service mix, capital allocation, geographic distribution and facility size.
- When designing facilities, keep costs down by reconsidering luxuries, high end finishes and oversized lobbies, but also oversized exam rooms and operating rooms where every square foot adds cost and reduces margins. The 2014 Guidelines allow for ambulatory OR’s as small as 250 SF (depending on the surgery to be performed there). Private for-profit ambulatory providers already plan their facilities this way.
- Efficiently program both the facility and the operations through lean planning and operational planning.
- Lobby to eliminate unnecessary “required” program spaces. In Certificate of Need (CON) states, waivers would need to be submitted but imaginative interpretations of the FGI Guidelines are usually seriously considered by AHJs if the reasoning is sound.
- If it is too late and your facility is built or near completion (but not occupied), look to re-purpose under-utilized space or non-revenue generating space (like offices).
- Regarding the real estate these facilities will occupy, look to repurpose existing under-utilized facilities you already control in lieu of building new and look for attractive leases.
- Health systems are looking to centralize their services as they continue to consolidate. This approach may also be applied to off-site facilities instead of building non-revenue generating support services into these locations; look to service them from system centralized locations if capacity can handle it.
- Revisit equity developer solutions as a way to defer first costs.

On the other side of reducing costs, consider adding beds to the facility and making it into the minimum requirements for a hospital. North Shore LIJ (now NorthWell Health) for their Lenox Hill Healthplex in New York City designed the facility as a 2-bed hospital, which allowed the free-standing emergency department (with a comprehensive care center above it) to be approved by the New York State Department of Health which was not a legislated facility type in New York State at the time. It would remain to be seen if that 2-bed scenario would comply with the wording of this new federal legislation just as the cost impacts of the added program would need to be studied to determine if it positively influences the ROI of the facility. It would seem to make sense in larger facilities where the added cost is a smaller percentage of the overall facility first cost.
Facility operations are another source for cost reduction, particularly optimizing operating and capital expenditures. As national systems grow larger through consolidation, they are looking for dedicated and variable resources to manage their healthcare facilities by applying technology, compliance understanding, procurement leverage and energy and sustainability initiatives to enhance value, streamline operations, and reduce operating expenses. This is accomplished by leveraging economies of scale, identification of waste and abuse, reengineering the work process, better financial controls, higher utilization of specialized skills and equipment, more efficient work process, performance based contracts and right-sizing the work force.
CONCLUSION
As the impact of this new legislation is felt by healthcare providers around the country, new solutions will evolve that will test its limitations. Healthcare facilities managers, designers and builders can help these efforts by evaluating trends and providing creative solutions.
About the Author: Charles Maggio has over 31 years of experience having worked as a practicing architect, hospital facilities executive, project manager and consultant. His architectural background and consulting expertise allow him to evaluate challenges and develop strategic solutions that position clients for success in today’s dynamic healthcare market. Charles leads CBRE Healthcare’s northeast team providing hospitals and health systems in the region an integrated platform of services. Charles is currently a member of the 2018 Health Guidelines Revision Committee Sheering and was formerly on the 2014 Health Guidelines Revision Committee for Design & Construction of Healthcare Facilities. He holds a Bachelor of Architecture from City University of New York City College.

Related Stories
Giants 400 | Jan 15, 2024
Top 130 Hospital Facility Architecture Firms for 2023
HKS, HDR, Stantec, CannonDesign, and Page Southerland Page top BD+C's ranking of the nation's largest hospital facility architecture and architecture engineering (AE) firms for 2023, as reported in the 2023 Giants 400 Report.
Healthcare Facilities | Jan 7, 2024
Two new projects could be economic catalysts for a central New Jersey city
A Cancer Center and Innovation district are under construction and expected to start opening in 2025 in New Brunswick.
Designers | Jan 3, 2024
Designing better built environments for a neurodiverse world
For most of human history, design has mostly considered “typical users” who are fully able-bodied without clinical or emotional disabilities. The problem with this approach is that it offers a limited perspective on how space can positively or negatively influence someone based on their physical, mental, and sensory abilities.
Healthcare Facilities | Dec 19, 2023
A new hospital in Duluth, Minn., is now the region’s largest healthcare facility
In Duluth, Minn., the new St. Mary’s Medical Center, designed by EwingCole, is now the largest healthcare facility in the region. The hospital consolidates Essentia Health’s healthcare services under one roof. At about 1 million sf spanning two city blocks, St. Mary’s overlooks Lake Superior, providing views on almost every floor of the world’s largest freshwater lake.
Healthcare Facilities | Dec 7, 2023
New $650 million Baptist Health Care complex opens in Pensacola
Baptist Health Care’s new $650 million healthcare complex opened recently in Pensacola, Fla. Featuring a 10-story, 268-bed hospital, the project “represents the single-largest investment in the healthcare history of northwest Florida,” said Gresham Smith project executive Robert “Skip” Yauger, AIA, LEED AP. The 602,000 sf Baptist Hospital is equipped with a Level II trauma center that provides 61 exam rooms and three triage areas.
Engineers | Nov 27, 2023
Kimley-Horn eliminates the guesswork of electric vehicle charger site selection
Private businesses and governments can now choose their new electric vehicle (EV) charger locations with data-driven precision. Kimley-Horn, the national engineering, planning, and design consulting firm, today launched TREDLite EV, a cloud-based tool that helps organizations develop and optimize their EV charger deployment strategies based on the organization’s unique priorities.
Healthcare Facilities | Nov 3, 2023
The University of Chicago Medicine is building its city’s first freestanding cancer center with inpatient and outpatient services
The University of Chicago Medicine (UChicago Medicine) is building Chicago’s first freestanding cancer center with inpatient and outpatient services. Aiming to bridge longstanding health disparities on Chicago’s South Side, the $815 million project will consolidate care and about 200 team members currently spread across at least five buildings. The new facility, which broke ground in September, is expected to open to patients in spring 2027.
Sponsored | | Oct 17, 2023
The Evolution of Medical Facility Security
As the healthcare system grows, securing these facilities becomes ever more challenging. Increasingly, medical providers have multiple facilities within their networks, making traditional keying systems and credentialing impractical.
Healthcare Facilities | Oct 11, 2023
Leveraging land and light to enhance patient care
GBBN interior designer Kristin Greeley shares insights from the firm's latest project: a cancer center in Santa Fe, N.M.
Healthcare Facilities | Oct 9, 2023
Design solutions for mental health as a secondary diagnosis
Rachel Vedder, RA, LEED AP, Senior Architect, Design Collaborative, shares two design solutions for hospitals treating behavioral health patients.