Many of us value the personal experience of a one-on-one encounter with our primary care physician. Developing a relationship with a single caregiver who is familiar with your medical history is reassuring and represents the traditional vision of care, for both patients and physicians. But more of us also value the convenience of online appointment scheduling, 24 hour nursing consultation by phone, and having our medical records including medication history, scans, X-rays, and visit summaries available at any time on secure websites. We are growing more comfortable with the digital realm, and with limiting our actual visits with our doctors to periodic physical exams and urgent medical needs.
Telemedicine
Telemedicine is a broad term that covers many aspects and mediums of care, but primarily it refers to the use of video monitors to allow a virtual face to face consultation to take place. Originally conducted in clinical settings to provide access to primary care or more commonly specialty care for people who may be located remotely or in a disadvantaged community without access to a local hospital or regular doctor, it has now expanded to encompass home sessions via face time or other programs on our tablets and phones. Initial reservations about the impersonal nature of such an encounter have largely given way to wide acceptance. Many patients actually feel they get more attention, more eye contact, with their physician via telemedicine than they do in an exam room where the physician spends a lot of time facing a separate monitor, typing notes directly into the patient’s electronic medical record (EMR).
Historic Drivers
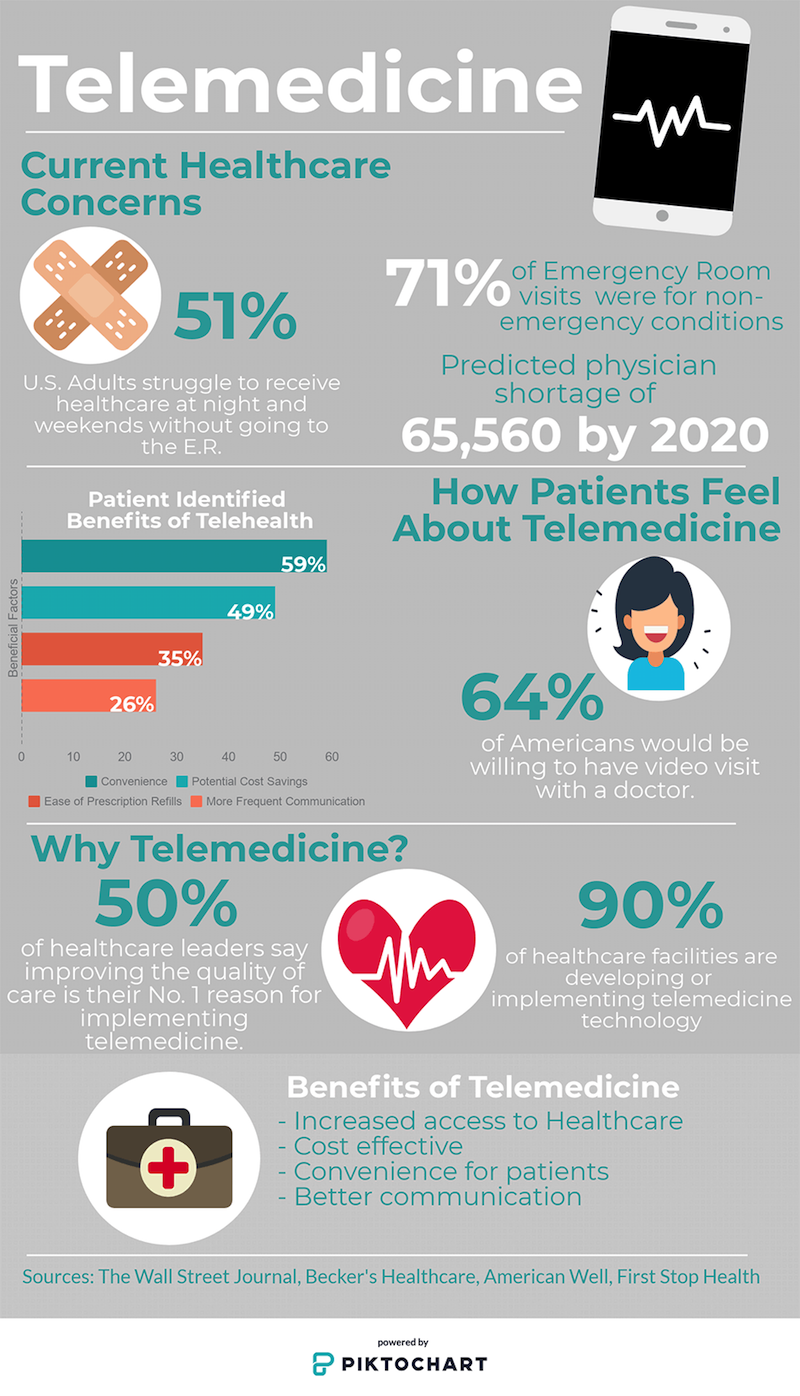
The increasing use of telemedicine is tied directly to the challenges of healthcare nationally; unsustainable rising costs of healthcare, a shortage of doctors and nurses available to provide care, and increasing levels of poor health and chronic conditions in the general population due to aging or lack of regular care. Early adoption by rural communities was driven by necessity as many of these populations are older, sicker and poorer compared to their urban counterparts, or the population as a whole. Telemedicine represents the ability to efficiently provide effective consultation and diagnosis without incurring the cost and inconvenience of travel, maintaining unnecessary numbers of physical exam rooms, or staffing full time positions in remote locations where they may be under-utilized. As primary care physicians and nurses age out of the workforce at a rate not currently being replenished, telemedicine expands the reach of those remaining and new providers coming into the system. Ultimately the ease and low cost of the telemedicine encounter promotes more comprehensive care, early diagnosis and intervention of potentially chronic conditions, and better follow-up care during rehabilitation to reduce readmissions after hospitalization.
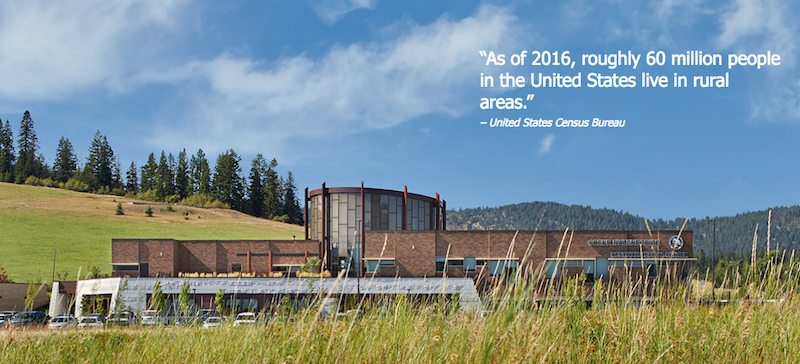 Marimn Health, Plummer, Idaho - NAC Architecture.
Marimn Health, Plummer, Idaho - NAC Architecture.
The Future of Telemedicine
The future of telemedicine is rapidly growing beyond the videoconference encounter as technology becomes more sophisticated. Micro cameras the size of a pill can now be swallowed by a patient and returned for a digital image of the gastrointestinal tract without the discomfort of a scope procedure. Home monitoring via digital wearables, originally targeted to fitness buffs, are now being used to track blood pressure, heart rate and other indicators for patients rehabbing at home. In the future smart phone-compatible, insertable heart monitors will track cardiac functions even more precisely, and diagnose the data for quicker cardiac event response. Today it is possible to take a picture of a blemish and use an app to process the image and provide a diagnosis of the skin condition. Pocket sized ultrasound devices the size of an electric shaver can detect subdermal potentially cancerous growths too small to otherwise feel. All of these developments point to the growing ability of patients to self-diagnose and consult with their physician via a digital encounter without the need of a clinical visit.

What Does This Mean For Architecture?
For the last few decades patient care has been transitioning away from hospitalization to ambulatory and clinical care; from expensive acute inpatient environments to less expensive outpatient settings. There will always be a need for operating rooms and intensive care wards (whether staffed by people or robots) but the quantity of such environments is declining and hence the need for specialized medical design expertise may be less in demand. Outpatient clinical environments tend to be simpler with design driven more by efficiency and branding, responding to the consumer’s preference for convenience and the providers’ desire to expand and protect market share. This tends to favor design firms that can develop prototype clinical models for wide implementation which feature a hospitality style that reinforces the provider’s identity.
But if it is no longer necessary for patients to visit the clinical environment for basic diagnosis of simple and even complex conditions, will the need for clinic facilities decline as well? What is the long term future of healthcare design? The answer may be in how architects are able to distill their medical expertise into more efficient delivery of acute care facilities, and anticipate the evolution of environments that support the delivery of telemedicine. Regarding efficiency, the healthcare industry and medical designers have adopted the tools of lean production to constantly improve the delivery of care and the quality of the care environment. The development of 3-party agreements and Lean Integrated Project Delivery (ILPD) have streamlined the delivery process by bringing the client, architect and builder into an integrated team focused on the best possible facility designs built in the shortest amount of time with the lowest cost. All stakeholders see the advantages of this approach.
 Mercy Virtual Care Center, Chesterfield, Missouri, by Forum Studio.
Mercy Virtual Care Center, Chesterfield, Missouri, by Forum Studio.
The future of clinic facilities design may depend on how architects are able to anticipate the evolution and delivery of telemedicine.
The more interesting prospect may be to see how new designs emerge to address the needs of both patients and practitioners engaging in telemedicine encounters and sharing data. I am looking forward to seeing environments, fixed or mobile, designed to enhance the remote encounter experience for the patient beyond what can happen at home. Universally, excellent lighting with natural color correction will increase the accuracy of diagnosis and an elevated level of acoustic separation will minimize distractions and instill confidence in the privacy of the discussion. Consultation rooms can be further tailored to serve distinct populations such as pediatric, geriatric and behavioral health patients, incorporating colors and cues to reduce anxiety and promote calm. With comfortable appointments and high resolution technology the conversation could feel as if you are sitting in the room with your doctor rather than just talking through a screen
 Mercy Virtual Care Center, Chesterfield, Missouri, by Forum Studio.
Mercy Virtual Care Center, Chesterfield, Missouri, by Forum Studio.
And let’s not forget the providers. It would be a disservice to not design effective and inspiring environments for the physicians who may be spending a good part of their day, if not all of it, interacting with their patients electronically. Striking a balance between onstage digital engagement and offstage renewal will be key. Just such a project was recently built for Mercy Virtual in Chesterfield, Missouri. The facility has no patient areas. It was designed completely around the delivery of telemedicine with technology rich pods that support highly connected encounters. This new paradigm space is contained within a building that also features abundant collaborative settings and celebrates the surrounding natural environment with framed views from comfortably appointed break rooms. Mercy Virtual recently won an AIA healthcare design award for its sensitive balance of the physicians’ virtual needs and their physical quality of life.
In summary telemedicine, developed out of necessity to expand services to remote or disenfranchised communities, is now becoming more the norm. All healthcare providers large and small need to engage in the economic and health benefits digital practice offers. As an architect I see a bright future with expanding opportunities to create new environments and deliver them more efficiently. As a healthcare consumer, I look forward to the rewards of better health and wellness and lower cost that telemedicine and related technologies mean for me and my family.
More from Author
NAC Architecture | Apr 11, 2024
The just cause in behavioral health design: Make it right
NAC Architecture shares strategies for approaching behavioral health design collaboratively and thoughtfully, rather than simply applying a set of blanket rules.
NAC Architecture | Jan 26, 2023
6 ways 'choice architecture' enhances student well-being in residence halls
The environments we build and inhabit shape our lives and the choices we make. NAC Architecture's Lauren Scranton shares six strategies for enhancing well-being in residence halls.
NAC Architecture | Aug 4, 2022
Faculty housing: A powerful recruitment tool for universities
Recruitment is a growing issue for employers located in areas with a diminishing inventory of affordable housing.
NAC Architecture | Feb 24, 2020
Design for educational equity
Can architecture not only shape lives, but contribute to a more equitable and just society for marginalized people?
NAC Architecture | Aug 22, 2019
Holistic wellness: What we can learn from Native American healthcare practices
Are there existing organizations that have already addressed some of these issues that we can study and learn from?
NAC Architecture | Dec 7, 2018
Planning and constructing a hybrid operating room: Lessons learned
A Hybrid operating room (OR) is an OR that is outfitted with advanced imaging equipment that allows surgeons, radiologists, and other providers to use real-time images for guidance and assessment while performing complex surgeries.
NAC Architecture | Nov 7, 2018
Designing environments for memory care residents
How can architecture decrease frustration, increase the feeling of self-worth, and increase the ability to re-connect?
NAC Architecture | Oct 8, 2018
One size doesn't fit all: Student housing is not a pair of socks
While the programming and design for these buildings all kept a holistic living/learning experience at the core, they also had amazingly different outcomes.
NAC Architecture | Sep 12, 2018
Security vs. 21st century learning: We shouldn’t have to choose
In order to effectively talk about school design, we need to start by understanding what a school is designed to do.
NAC Architecture | Jul 6, 2018
Building for growth: Supporting gender-specific needs in middle school design
Today, efforts toward equity in education encompass a wide spectrum of considerations including sex, gender identity, socio-economic background, and ethnicity to name a few.