Several states and municipalities are aggressively investigating the conversion of hotels into makeshift hospitals in order to free up much-needed beds in hospitals for patients who have contracted COVID-19.
Leo A Daly is currently negotiating with several hoteliers about converting large portfolios of hotels into healthcare facilities that follow the firm’s Hotel2Hospital prototype, which would conform with design guidelines released last week to state governments by the U.S. Army Corps of Engineers, which relax some of the hospital safety standards.
The Nebraska-based firm is working with several national design-build contractors to get such conversions started.
“Hospitals and hotels have several common characteristics that make this a promising solution,” says Joshua Theodore, ACHE, EDAC, vice president and global health practice leader for Leo A Daly. “Both are comprised of private, individual rooms with a dedicated toilet and HVAC systems. Air handling is critical to patient and staff safety in infectious disease environments, so hotel rooms have an instant advantage over other typologies in terms of viability.”
Leo A Daly did not disclose the healthcare systems or contractors it is speaking or working with about its conversion proposals.
Three modes for hotel-to-hospital conversions for COVID-19
The average hotel could accommodate up to 80 patients, Leo A Daly estimates. And many are located near existing hospitals.
Hotels also have food service, cleaning service, waste removal and laundry service, all of which are critical to any inpatient healthcare facility, says Theodore. He notes, too, that hotels are currently experiencing high vacancy rates that are likely to persist until the coronavirus dissipates.
Hotel2Hospital offers three adaptive reuse models. Each will require different levels of biocontainment and intervention to the physical building.
Reuse Model 1 would be to quarantine suspected or asymptomatic COVID-19 patients. Reuse Model 2 would be for symptomatic isolation of patients with underlying risk factors who are already sick but aren’t likely to require full ICU inpatient treatment. (Ventilators and telemetry would likely be used for this facility type). Reuse Model 3 would be for non-infected patients who currently are being hospitalized and could potentially receive treatment in alternative care environments so as to free up hospital beds for more acute COVID-19 patients.
For Reuse Model 1, the hotel furniture could be used, but the bed would require medical linens. A nurse station would be created in a room opposite the elevator core, and the floor would also have an eye/hand washing station. In this model, the reception and office areas in the lobby would be repurposed for patient check-in. Any retail area would be converted to a pharmacy. And offices could be converted to lab space. The converted room would also need to be modified with a larger exhaust fan system to its existing toilet exhaust duct system to create negative pressure.
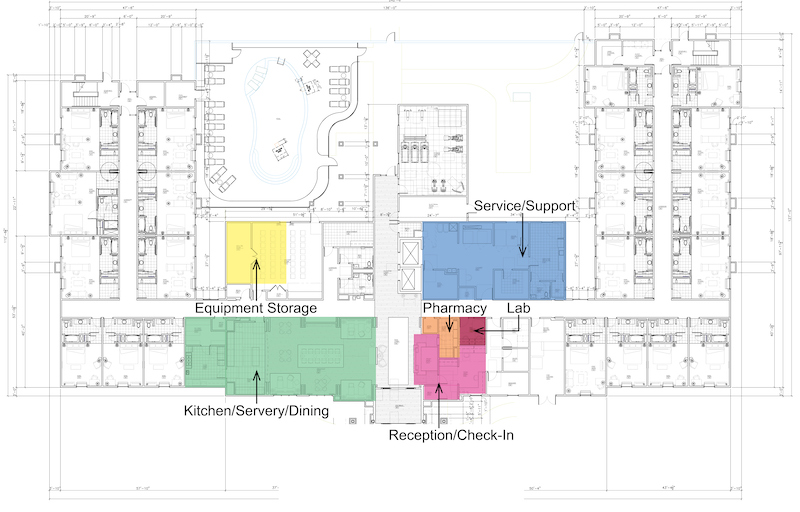
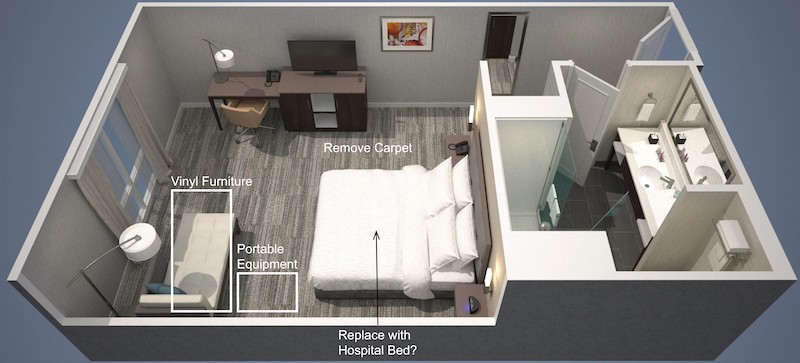
The Reuse Model 2 would, among other changes, convert the hotel's reception area into a patient check-in, and make retail and office spaces into pharmacies and labs. The carpeting in the rooms and corridors would be removed.
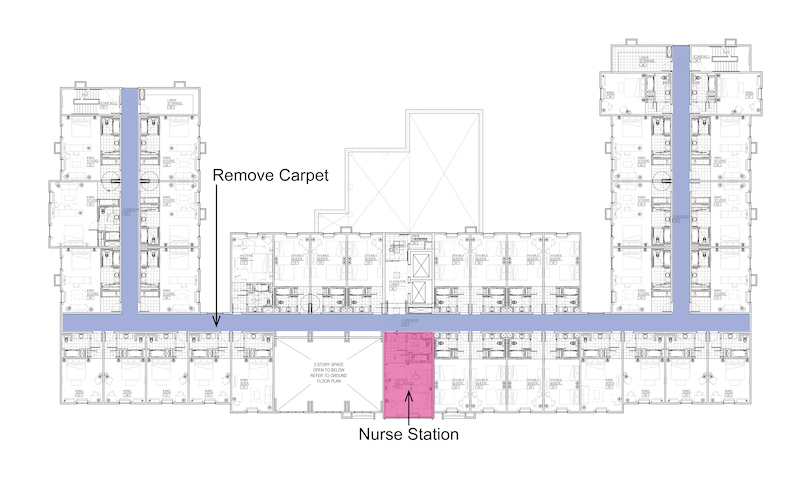
A conversion of a hotel to Reuse Model 2 would undertake the measures spelled out for Reuse Model 1, and then some. Carpeting, polishes, and concrete floor sealing would be removed from the rooms and corridors. Hospital-grade vinyl would replace fabric on furniture. Curtains would be replaced with motorized shade systems. Mobile headwall units and portable med gas bottles would be installed, as would electronic wireless patient surveillance and monitoring devices. The converted hotel would also need to create storage areas for portable medical equipment. (Medical gases would have to be portable.)
Reuse Model 3 would require all of the modifications described in Reuse Models 1 and 2. Leo A Daly suggests that exhaust modifications may not be necessary in all rooms. But infrastructure changes would include providing an exterior emergency generator system and transfer switch equipment for connection to the building’s power infrastructure. The IT infrastructure would be upgraded. Treatment and procedure spaces would be identified and equipped with recirculating HEPA filtration units to increase the room’s air changes per hour.
Theodore acknowledges that the Hotel2Hospital prototype conversions would need to address challenges that include staffing, HVAC, building codes, medical equipment management, the building’s power infrastructure, and meeting cleaning/support standards.
He says that Leo A Daly’s design teams have been meeting with hospitals, federal officials, developers and hotel owners to work through these complexities
Related Stories
Augmented Reality | Jan 27, 2023
Enhancing our M.O.O.D. through augmented reality therapy rooms
Perkins Eastman’s M.O.O.D. Space aims to make mental healthcare more accessible—and mental health more achievable.
K-12 Schools | Nov 30, 2022
School districts are prioritizing federal funds for air filtration, HVAC upgrades
U.S. school districts are widely planning to use funds from last year’s American Rescue Plan (ARP) to upgrade or improve air filtration and heating/cooling systems, according to a report from the Center for Green Schools at the U.S. Green Building Council. The report, “School Facilities Funding in the Pandemic,” says air filtration and HVAC upgrades are the top facility improvement choice for the 5,004 school districts included in the analysis.
Giants 400 | Nov 14, 2022
4 emerging trends from BD+C's 2022 Giants 400 Report
Regenerative design, cognitive health, and jobsite robotics highlight the top trends from the 519 design and construction firms that participated in BD+C's 2022 Giants 400 Report.
Healthcare Facilities | Jun 20, 2022
Is telehealth finally mainstream?
After more than a century of development, telehealth has become a standard alternative for many types of care.
Coronavirus | May 20, 2022
Center for Green Schools says U.S. schools need more support to fight COVID-19
The Center for Green Schools at the U.S. Green Building Council released a new report detailing how school districts around the country have managed air quality within their buildings during the second year of the COVID-19 pandemic.
Industry Research | Mar 9, 2022
Survey reveals five ways COVID-19 changed Americans’ impressions of public restrooms and facilities
Upon entering the third year of the pandemic, Americans are not only more sensitive to germs in public restrooms, they now hold higher standards for the cleanliness, condition and technology used in these shared spaces, according to the annual Healthy Handwashing Survey™ from Bradley Corporation conducted in January.
Codes and Standards | Feb 21, 2022
New standard for ultraviolet germicidal irradiation
The Illuminating Engineering Society (IES) recently introduced the standard, ANSI/IES RP-44-21 Recommended Practice: Ultraviolet Germicidal Irradiation.
Coronavirus | Jan 20, 2022
Advances and challenges in improving indoor air quality in commercial buildings
Michael Dreidger, CEO of IAQ tech startup Airsset speaks with BD+C's John Caulfield about how building owners and property managers can improve their buildings' air quality.
Coronavirus | Jul 20, 2021
5 leadership lessons for a post-pandemic world from Shawmut CEO Les Hiscoe
Les Hiscoe, PE, CEO of Shawmut, a $1.5 billion construction management company headquartered in Boston, offers a 5-point plan for dealing with the Covid pandemic.
Resiliency | Jul 15, 2021
A new report urges federal investment in healthier buildings
The National Institute of Building Sciences also calls for code changes and greater cooperation between building owners and the AEC community.