Healthcare consumers are just as likely to factor in convenience as they do cost when deciding where to seek care and from whom, according to a new survey of 4,037 American adults about their attitudes and preferences as patients.
The survey, conducted from April 19-28 by JLL, in many ways confirms the obvious: that older generations seek preventive care more often than younger generations; that insurance coverage is a primary driver for choosing a provider or hospital; and that the quality of service affects the patient experience.
Nearly eight of 10 of the survey’s respondents had received at least one type of non-dental care in the last year. Women, who accounted for 51% of the survey’s respondents, are more likely to receive care overall, but men are more likely to receive emergency care.
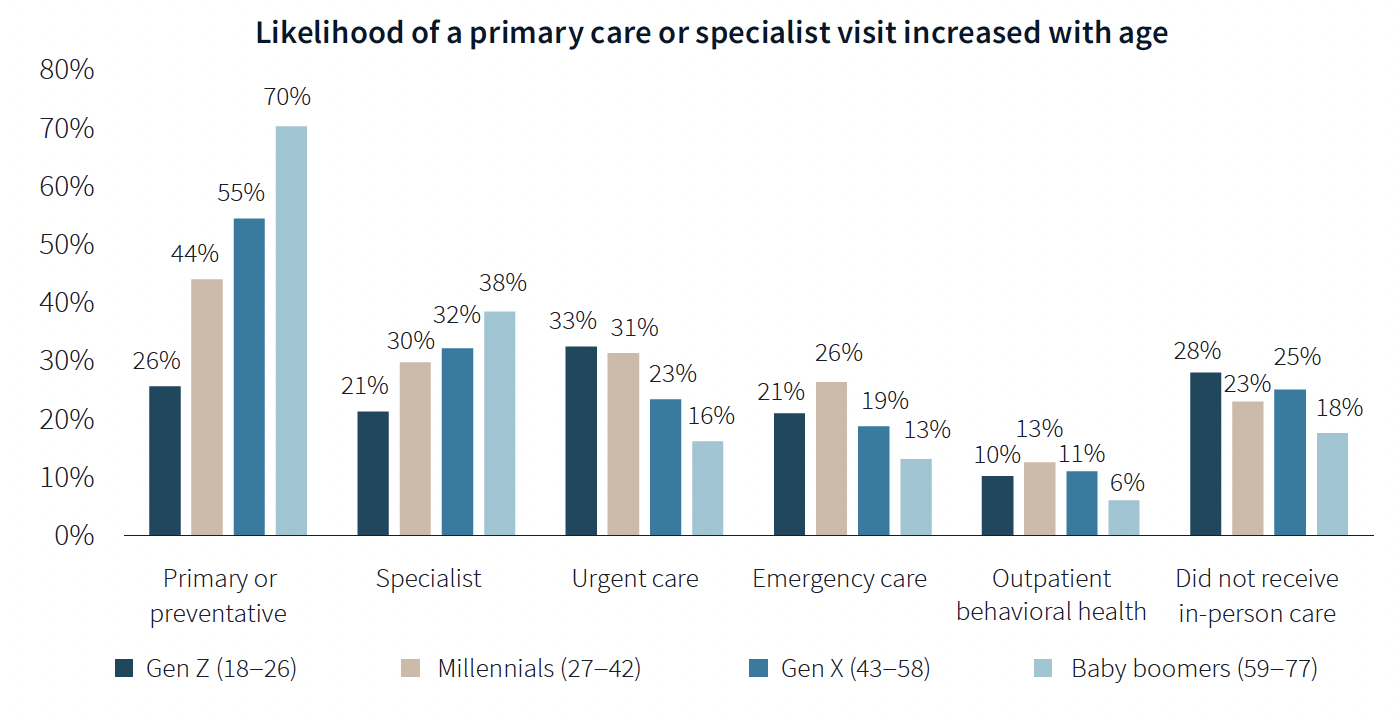
The likelihood of a primary care or specialist visit increases with age: 80% of adults 65 years or older have two or more chronic conditions that require continuous care. More than 70% of Baby Boomers (who accounted for 29% of the survey’s respondents) had received primary or preventive care within the last year, compared to only 26% of Generation Z.
Younger generations are more reactive than preventive in their healthcare decisions, borne out by the survey’s finding that Millennials and Gen Zs (43% of the survey's respondents) are more likely to receive urgent care, emergency care, and outpatient behavioral healthcare than older adults.
Proximity to patients counts
When care is urgently needed, “decision factors are simplified,” the survey states, and location and proximity of care are ranked higher as decision-making factors. But even outside of emergencies, convenience ranks high among factors for patients seeking care.
There’s no denying that cost is always in the background of any healthcare decision. “Accept my insurance” was the most common factor for choosing a provider among the survey’s respondents. (82% of participants has private insurance, and 81% has public insurance.)
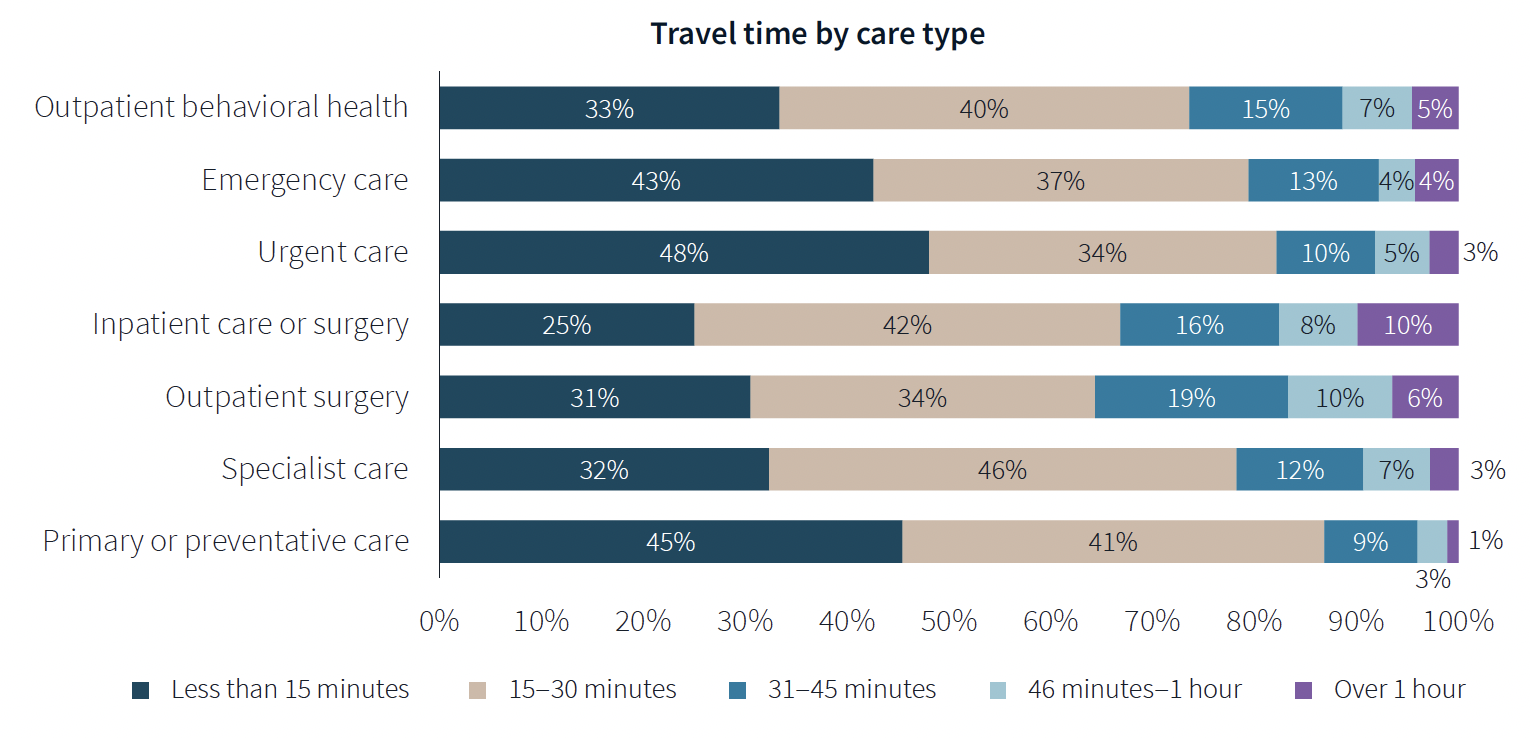
Two-fifths of respondents said they travel less than 15 minutes to receive care, and nearly eight of 10 respondents travel less than 30 minutes. Among those with appointments in standalone medical offices, 85% ranked location as convenience, which the survey suggested indicates the advantages of a dispersed location strategy.
“A strong location strategy can improve reach for health systems and physician practices and potentially improve care outcomes,” JLL writes. “But there is a balance between convenience and cost—health systems need to balance the benefits of being close to their target population with the cost of a new facility or doctors’ time in transit from a local clinic to the hospital.”
Convenience is also key both in location and in being able to navigate to care. Patients want to get to care quickly and get on with their day. Ease of parking and ability to navigate the facility also affected a facility’s net positive score in the survey.
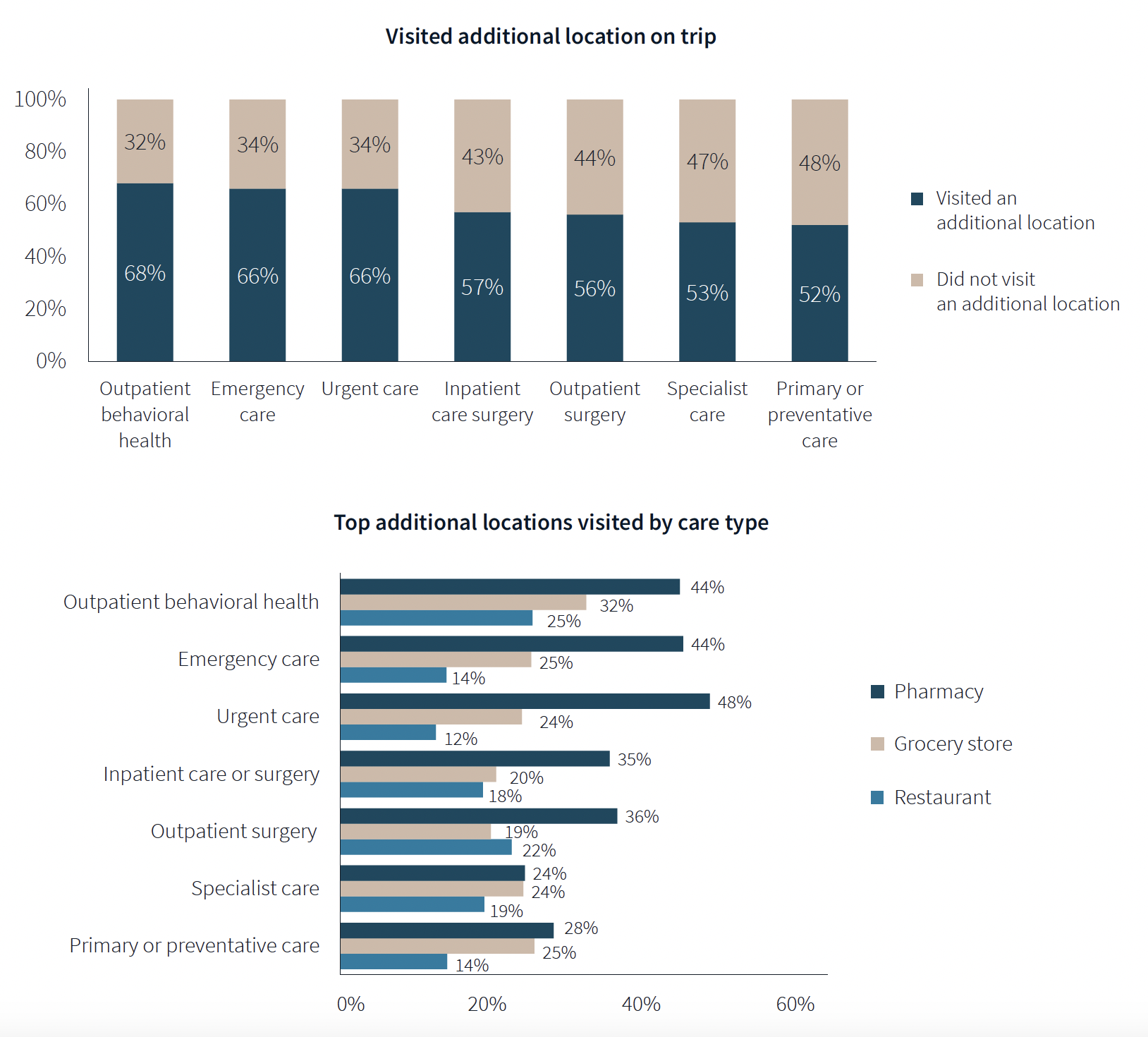
One of the survey’s more revealing findings is that nearly three-fifths of respondents—58%—went to another location—such as a pharmacy, or an urgent clinic—as part of their trip for healthcare.
Word of mouth often defines quality of care
Patients seem to be open to diverse care choices. For example, 29% said they have visited a retail clinic, such as a CVS, and would do so again. Gen Z and Millennials are more likely to frequent retail clinics for their convenient appointment schedules and shorter wait times.
More than two-fifths of respondents—42%—had a telehealth appointment within the last year, which was slightly down from the 45% in JLL’s 2022 survey. This year’s poll also found that 29% of telehealth appointments led to an in-person visit.
More than 40% of respondents ranked “reputation of quality” among the top five factors for choosing care. But where they get their impressions about quality varies.
Referrals play a larger role in specialist, outpatient surgery and inpatient care. Recommendations from friends ranked most highly for behavioral health, given the personal nature of such care, and was ranked in the top five by 31% of respondents. Younger patients, who “have yet to develop brand loyalty,” according to the survey, are more likely to rely on word-of-mouth recommendations than older patients for whom hospital systems’ reps matter more.
Outpatient surgery and primary care ranked highest for provider satisfaction; emergency care ranked lowest. Participants ranked their experiences on 12 aspects of care, and the biggest gap between “promoters” and “detractors” was for the service level of providers. Primary care had the highest net provider score, with 86% of respondents ranking its care as “attentive.”
Some amenities draw patients
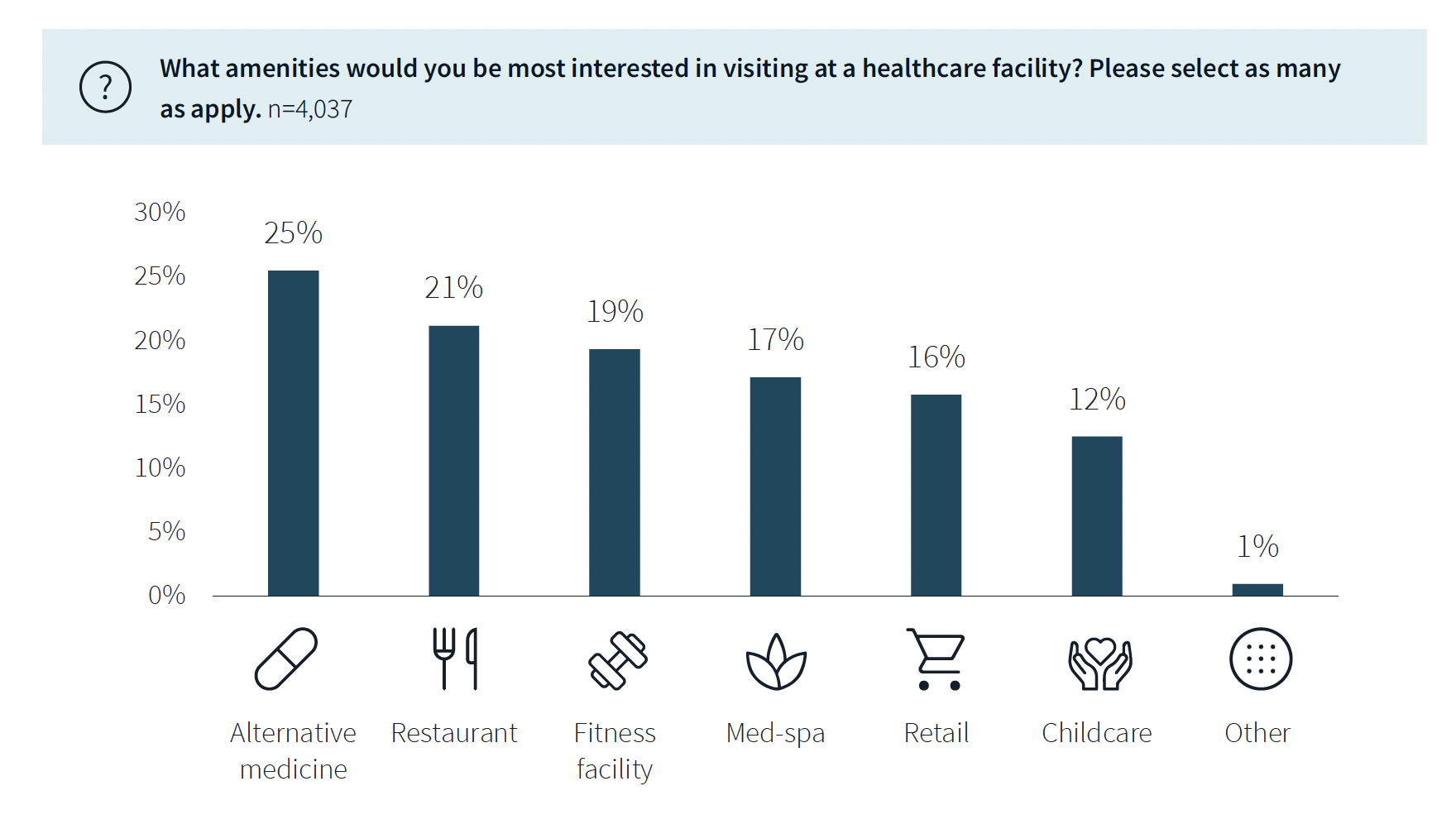
While not a decision-making factor, amenities do attract some patients. Among the survey’s respondents, 63% said they would be interested in visiting a healthcare facility with an additional amenity, such as alternative medicine, a restaurant, fitness center, or spa. (This inclination was more evident among younger respondents.)
The overall quality of facilities, including the comfort of their waiting rooms, can impact a patient’s choice, especially for inpatient, urgent, and emergency care. The survey also found that urban locations have lower favorability rankings for their facilities, signaling room for improvement. (Just under half—48%—of respondents live in the suburbs.)
Related Stories
| Aug 16, 2022
Cedars-Sinai Urgent Care Clinic’s high design for urgent care
The new Cedars-Sinai Los Feliz Urgent Care Clinic in Los Angeles plays against type, offering a stylized design to what are typically mundane, utilitarian buildings.
| Aug 15, 2022
IF you build it, will they come? The problem of staff respite in healthcare facilities
Architects and designers have long argued for the value of respite spaces in healthcare facilities.
AEC Tech | Aug 8, 2022
The technology balancing act
As our world reopens from COVID isolation, we are entering back into undefined territory – a form of hybrid existence.
| Aug 3, 2022
Designing learning environments to support the future of equitable health care
While the shortage of rural health care practitioners was a concern before the COVID-19 pandemic, the public health crisis has highlighted the importance of health equity in the United States and the desperate need for practitioners help meet the needs of patients in vulnerable rural communities.
Healthcare Facilities | Aug 1, 2022
New Phoenix VA outpatient clinic is one of the largest veteran care facilities in the U.S.
The new Phoenix 32nd Street VA Clinic, spanning roughly 275,000 sf over 15 acres, is one of the largest veteran care facilities in the U.S.
Building Team | Jul 12, 2022
10 resource reduction measures for more efficient and sustainable biopharma facilities
Resource reduction measures are solutions that can lead to lifecycle energy and cost savings for a favorable return on investment while simultaneously improving resiliency and promoting health and wellness in your facility.
Healthcare Facilities | Jun 22, 2022
Arizona State University’s Health Futures Center: A new home for medical tech innovation
In Phoenix, the Arizona State University (ASU) has constructed its Health Futures Center—expanding the school’s impact as a research institution emphasizing medical technology acceleration and innovation, entrepreneurship, and healthcare education.
Healthcare Facilities | Jun 20, 2022
Is telehealth finally mainstream?
After more than a century of development, telehealth has become a standard alternative for many types of care.
Codes and Standards | Jun 14, 2022
Hospitals’ fossil fuel use trending downward, but electricity use isn’t declining as much
The 2021 Hospital Energy and Water Benchmarking Survey by Grumman|Butkus Associates found that U.S. hospitals’ use of fossil fuels is declining since the inception of the annual survey 25 years ago, but electricity use is dipping more slowly.
Healthcare Facilities | Jun 13, 2022
University of Kansas Health System cancer care floors foster community and empathy
On three floors of Cambridge Tower A at The University of Kansas Health System in Kansas City, patients being treated for blood cancers have a dedicated space that not only keeps them safe during immune system comprising treatments, but also provide feelings of comfort and compassion.

















