For the last 10 years or so, advocates of sustainable design have promoted its potential to enhance the health and wellness of building occupants, including hospital patients. In practice, projects seeking to link healthy outcomes and sustainable design have been limited in scope to such actions as reducing exposure to toxic chemicals for building occupants and construction workers.
LEED for Neighborhood Development and the Active Design Guidelines are notable exceptions to this trend. Both draw from population health research to promote strategies that reduce barriers to a healthy lifestyle.
It is my belief, however, that more can be done with the data we already have. In my view, contextual health data can provide a unique and valuable insight into the design process. It should be incorporated into the due diligence performed on any building project, much in the way we check the building code before starting to design.
Unfortunately, the path to more extensive use of health data in green building is blocked by certain myths that have to be debunked before such data can be successfully incorporated into the project delivery process. They are as follows:
1. There’s not enough data to support a direct link between design and health.
2. Population health considerations do not generate profit.
3. Population health data is not site-specific.
4. Community health is not the responsibility of building owners or developers, or their Building Teams.
5. Analyzing health data will slow down—and possibly jeopardize—the project.
Allow me to expose the flaws in each of these myths.
Myth #1: There’s not enough data to support a direct link between design and health.
This myth is based on a misunderstanding as to the quantity of population health data that is available to inform design. Skepticism with regard to environmental health studies is particularly strong in the medical field: physicians rely on a biomedical model based on randomized controlled trials before new drugs or treatments are approved for clinical use.
That methodology doesn’t work for health concerns linked to the environment, because it is not possible to isolate a single variable to prove that, say, a child’s asthma is most likely caused by a poorly maintained school facility. Other environmental factors may contribute, such as asthma triggers in the home, living near a freeway, high pollen concentration, or genetics.
But that doesn’t mean we should throw up our hands in despair. There is a massive body of public health research that has examined such questions as: Why is there such a high incidence of diabetes in certain neighborhoods? Why are there so many asthmatic children among certain populations? Why do more people die during heat waves in some neighborhoods than in others? Has the built environment contributed to these conditions? If so, how? Can we examine the data and work backwards to see if certain design strategies could help alleviate such negative health and wellness conditions?
Take the case of a medical center that is experiencing a spike in indigent patients flooding its emergency department. The traditional response might be: build a bigger ED. However, available data might show that the surrounding community has an unusually high percentage of asthmatic children and families without health insurance.
The wiser long-term approach would be for that medical center to go outside its walls and look at opportunities to reduce asthma triggers at home, at school, and in the community. The Affordable Care Act is encouraging health systems to start thinking this way through its focus on prevention and chronic disease.
Myth #2: Population health considerations do not generate profit.
The problem here is that, under the traditional fee-for-service model, sustainable improvements don’t directly benefit the party (usually the hospital) that’s paying the bill. In fact, they could backfire and actually reduce the hospital’s revenues.
Here again, the Affordable Care Act is playing a significant role in changing that model by tying Medicare and Medicaid reimbursements to health outcomes associated with chronic conditions that are expensive to treat—diabetes, heart disease, etc. By incorporating the environmental determinants underlying these diseases into the community health needs assessments that nonprofit medical systems are required to develop, changes in the built environment could be factored into future reimbursement mechanisms.

MD Anderson Cancer Center at Cooper, Camden, N.J. Photo: Chris Cooper / courtesy Francis Cauffman
Some integrated health systems have already seen the financial benefits of taking this approach. Kaiser Permanente’s Community Health Initiative uses mapping technology to pinpoint geographic areas with high concentrations of, say, people with diabetes. Using a combination of their internal health data and environmental data, KP can combine traditional clinical care with public health efforts, such as education on healthy eating and active living programs that modify the built environment—for example, constructing walking trails in affected neighborhoods.
Myth #3: Population health data is not site-specific.
Proponents of this myth assume that population health data cannot be gathered at a sufficiently granular level to be relevant to a specific building project. That does not mean it is impossible to gather data that could be applied at the individual building project level; in fact, reams of such data already exist and are waiting to be used.
For legal, ethical, and privacy reasons, health-related data on people—hospital patients, kindergartners, college students—has to be aggregated. Nobody wants individual health records to go public. But healthcare is already one of the most data-intensives sectors of the economy. Healthcare providers know a lot about you and me.
With the coming proliferation of electronic medical records, they’re going to have even more “big data” to work with, at least internally. As that information becomes available (on an aggregated basis, of course) to healthcare design teams, it will become an invaluable resource for planning and decision making at even the most site-specific scale.
Myth #4: Community health is not the responsibility of building owners or developers, or their Building Teams.
Private-sector building owners and developers usually are not compelled to justify the impact of their projects on the community, particularly if there are any potential negative effects on health or human welfare. True, some developers may use an aspect of “community betterment” as a marketing tool for their projects. But most developers want to avoid making any claims as to the health benefits of their green buildings, for fear they might one day have to live up to such claims in court.
An example of the trend toward using wellness as a development’s theme is the Jackson Walk mixed-use project in Jackson, Tenn. The development, which combines office, retail, and residential components, is anchored by a combined fitness center, wellness center, and outpatient clinic called LIFT (Living in a Fit Tennessee).
The healthcare industry has led the building sector for a number of years in highlighting the value that thoughtful building design can bring to community health. For example, a number of nonprofit systems that participated in the Green Guide for Health Care best practices program gave special consideration to green design strategies that could be identified as fulfilling the IRS’s requirement for investing in practices that benefit community health.
In one case, a hospital worked with its local transit authority to expand bus service in the neighborhood surrounding the medical campus, a clear benefit to patients, their families, hospital staff, and the neighboring community. Other hospitals are putting in nature preserves or small parks that are open to the public, thereby encouraging wellness through exercise. Hospitals across the country have used on-site healthy food initiatives to increase access to healthy food for residents of surrounding communities.
Myth #5: Analyzing health data will slow down—and possibly jeopardize—the project.
It is true: traditional public health research almost always takes longer to produce than the schedule for a typical real estate or hospital construction project would allow. This makes it unlikely that any new, full-blown public health study could be conducted in time to influence the design of such a project.
What’s changing this picture is the confluence of greater availability of big data, new technologies, and faster assessment tools, all of which make it possible to radically shorten the timeframe needed to develop credible health-related design recommendations. This is especially true now that federal agencies—notably, Health and Human Services, which includes the Centers for Medicare & Medicaid Services and the Centers for Disease Control & Prevention—must (under a 2013 Executive Order) make government data “open and machine readable.”
With all that data flowing freely, you should be able to do your health-related due diligence without having to collect new data on your own. As you become more familiar with this process, you should be able to pull together the available data, analyze it, and make recommendations that could improve occupant health before the design has been set in stone. Such an assessment might even lead to suggested modifications in the community—improving sidewalks and reducing traffic congestion, for example—to redress unhealthy environmental conditions.
One important point here: Keep in mind that health data analysis is not primarily intended to introduce novel design strategies to a project. Rather, it should be used to prioritize strategies to meet the project’s goals, whether programmatic, operational, or related to sustainability concerns.
One tool that could be borrowed from the public health sector to apply health data to the design process is the health impact assessment. While HIAs are widely used in Europe and other parts of the world, they have only been in use in the U.S. for 15 years or so. They have experienced rapid growth here over the past few years due to the success of the national Health Impact Project—sponsored by the Robert Wood Johnson Foundation and The Pew Charitable Trusts—at promoting their use.
HIAs use a six-step, evidence-based process to identify the health consequences of a new policy or project and offer practical strategies to enhance its health benefits and minimize its adverse effects—including, presumably, green building. They take the mystery out of where health data comes from and how it can be effectively used to enhance the development process.
Many of the myths I have laid out here are starting to fade away as a result of major shifts in policy, technology, and culture: the Affordable Care Act, the advent of big data, a growing recognition of the built environment’s role in maintaining a healthy lifestyle, etc. It is up to the leaders in the building industry to flip these myths on their head by recognizing and capitalizing on the value that contextual health data brings to the design process.
Adele Houghton is President of Biositu, LLC, which provides evidence-based, data-driven consulting services to clients on topics related to green building, public health, and climate change. She is a Registered Architect and LEED Accredited Professional in Building Design + Construction, Operations + Maintenance, and Neighborhood Development. She holds a Master of Public Health and a Certificate in Public Health Informatics from Johns Hopkins University. From 2005-2008, she served as Pilot Project Coordinator and Project Manager of the Green Guide for Health Care.
Related Stories
High-rise Construction | Mar 16, 2015
NBBJ creates 'shadowless' skyscraper concept for proposed UK development
A team of architects from the London branch of NBBJ used computer algorithms to generate a dual-tower design that maximizes sunlight reflections to eliminate the buildings' shadows.
BIM and Information Technology | Mar 11, 2015
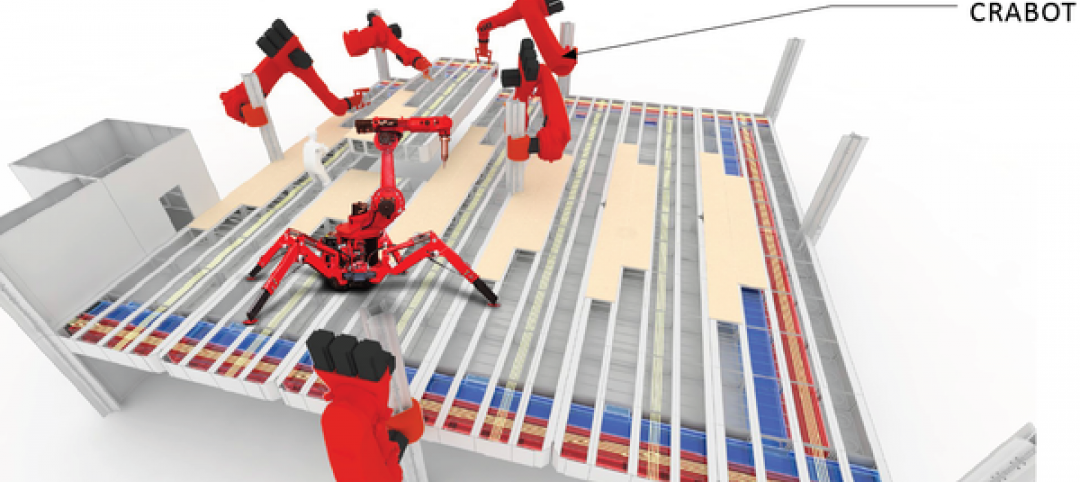
Google plans to use robots, cranes to manipulate modular offices at its new HQ
Its visions of “crabots” accentuate the search-engine giant’s recent fascination with robotics and automation.
Museums | Mar 5, 2015
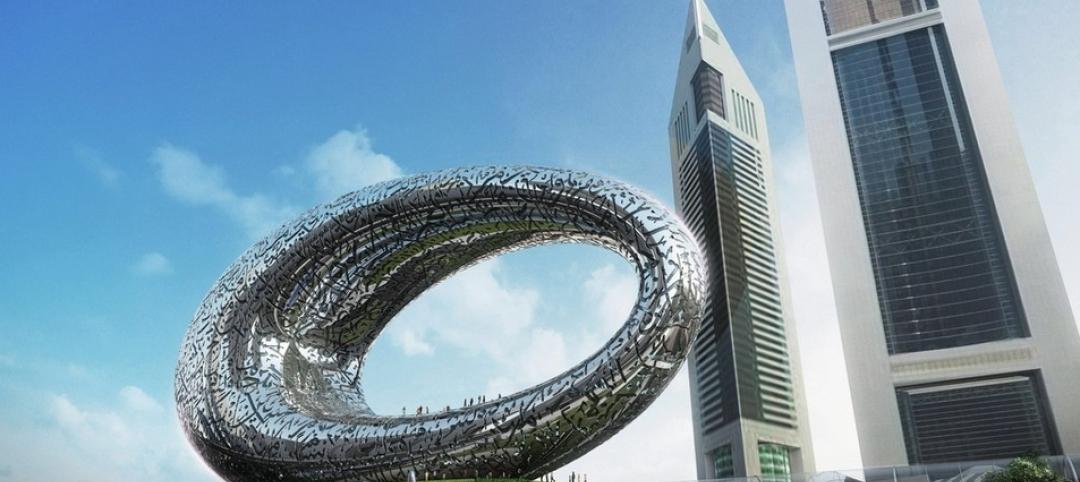
A giant, silver loop in Dubai will house the Museum of the Future
The Sheikh of Dubai hopes the $136 million museum will serve as an incubator for ideas and real designs—a global destination for inventors and entrepreneurs.
BIM and Information Technology | Mar 4, 2015
Why China's CCTV building needed a WiFi retrofit
It took a year-long retrofit to get WiFi transmission issues solved at China's iconic skyscraper.
Energy Efficiency | Mar 4, 2015
DOE launches crowdsourcing website for technology innovators
The Oak Ridge National Laboratory launched a new crowdsourcing website called the Buildings Crowdsoucing Community to collect and share ideas by innovators for energy-efficient technologies to use in homes and buildings.
Sponsored | BIM and Information Technology | Mar 3, 2015
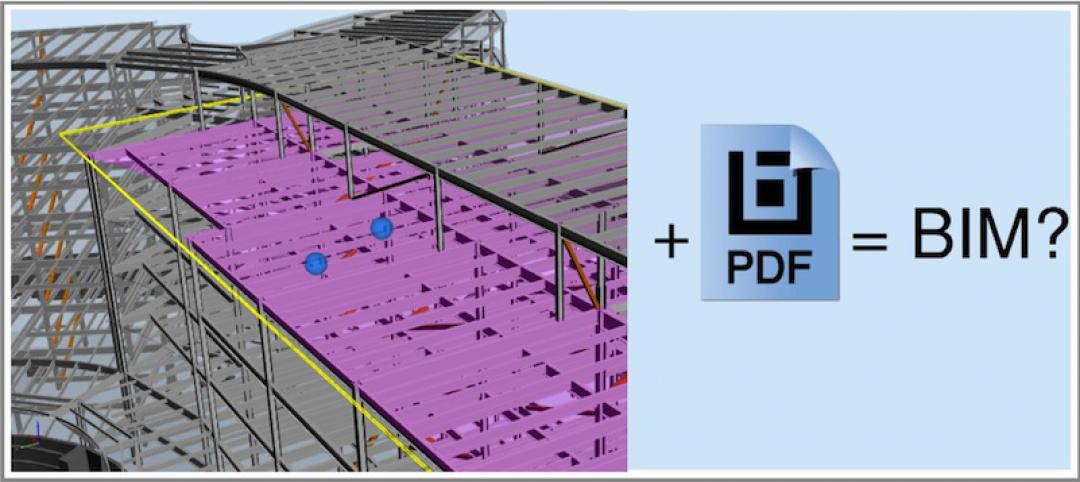
The great debate: Is 3D PDF really BIM?
You can pull apart buildings, cut through floors, and view simulated animation for assembly instructions all within a PDF.
BIM and Information Technology | Feb 23, 2015
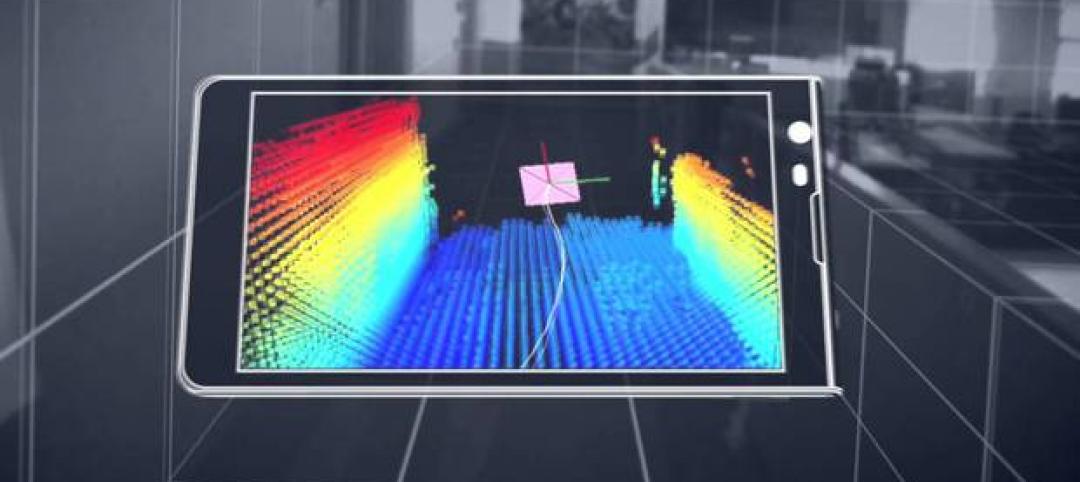
9 best practices for effective laser scanning
JE Dunn’s National BIM Director, Trent Nichols, offers tips and advice for mastering the art of laser scanning.
BIM and Information Technology | Feb 10, 2015
Google's 3D scanning camera leaves the lab
Google is said to be partnering with LG to create a version of the technology for public release sometime this year.
BIM and Information Technology | Feb 8, 2015
BIM for safety: How to use BIM/VDC tools to prevent injuries on the job site
Gilbane, Southland Industries, Tocci, and Turner are among the firms to incorporate advanced 4D BIM safety assessment and planning on projects.