Between five million and nine million Americans are expected to become infected with the coronavirus, one-third of whom might need intensive care. But there are only 920,000 staffed hospital beds in the U.S., according to the American Hospital Association.
To help fill that gap, stadiums and convention centers have become the focus of many alternate healthcare conversion strategies. There may be other solutions as well. The Army Corps of Engineers has looked at more than 800 existing buildings for possible conversion, nearly half of which are hotels. And the architecture firm HKS, in collaboration with MEP engineer Mazzetti, has released a concept study on how to convert a medium-to-large high school into functional patient care and sequestration space within 10 to 15 days. (The full report can be downloaded from here.)
The paper suggests that high schools are good conversion options because they are found in almost all communities, are big enough to house 200 to 500 COVIC-19 patients (depending on the size of the facility), have wide corridors and mostly nonporous durable surfaces for easy cleaning, are designed for adults (unlike elementary schools), have spaces that are easily convertible to patient care and support requirements, and would require minimal intervention for the conversion.
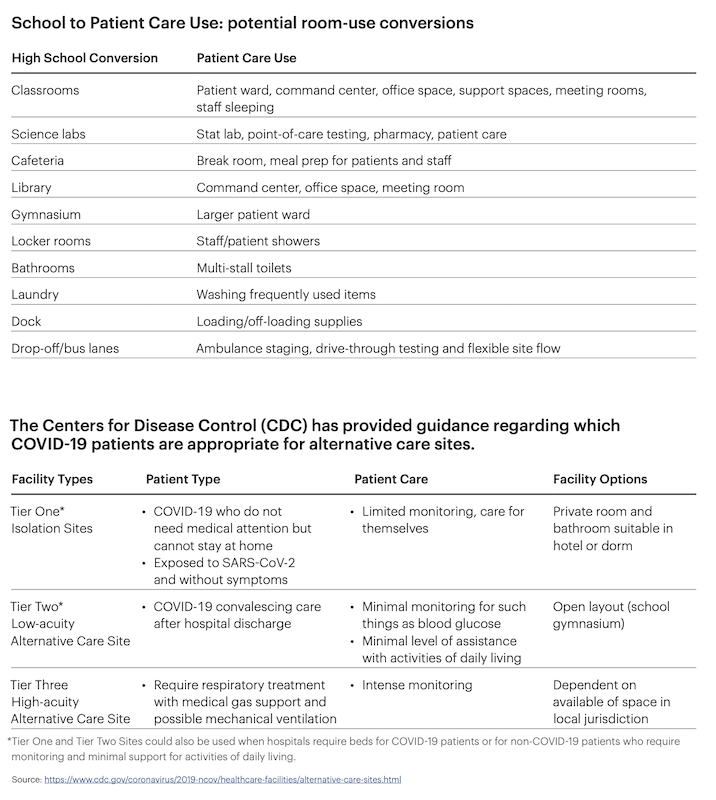
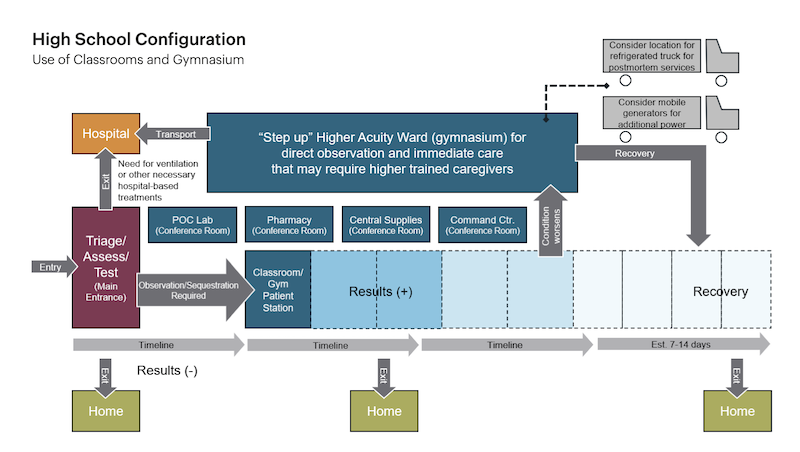
HKS believes that high schools could be converted to meet Tier 1 and 2 guidelines by the CDC.
The paper’s three authors believe that high schools can be converted to Tier 1 or 2 alternate care facilities, as defined by Centers for Disease and Prevention Control guidelines. The patients who would be most appropriate for a COVID-19 school stay are those who are suspected of being a carrier, confirmed positive but not exhibiting severe symptoms and/or can’t care for themselves, or are recovering from COVID-19 but still requiring care.
The patients would be ambulatory and would not need special ventilation, machine-assisted breathing or anything more than minimal oxygen assistance.
The paper assumes that some form of assessment, testing and/ or triage is happening on the school grounds. This could be drive-through testing. Now that quick tests (within an hour) are available, assessment and determination can be almost immediate.
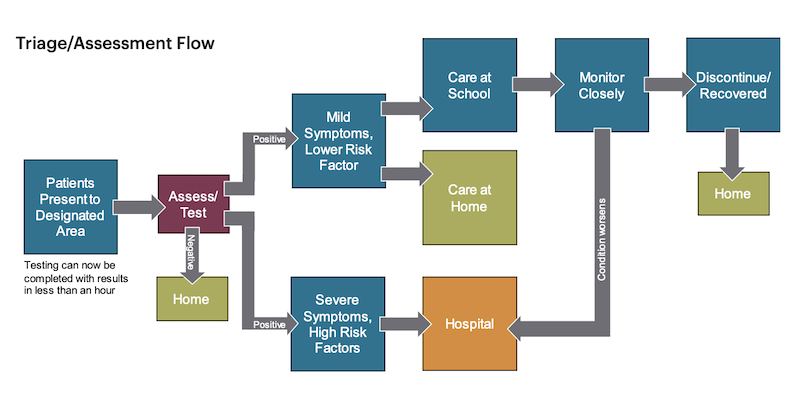
The concept assumes that there would be some kind of infection assessment and testing done onsite.
The paper provides a step-by-step process for converting both classrooms and gymnasiums. It states that converting classrooms for low-acuity patients “can be rather simple” with the following considerations:
- Remove non-essential furniture to allow for more caregiver space and patient beds/cots. Desks and tables can be moved to unused classrooms or ancillary buildings. If there is enough space in the room, desks may be used as bedside tables.
- Utilize features already in the classrooms, such as a telephone that connects to a central office, Wi-Fi connectivity, computers and overhead intercoms.
- Hospital beds would be optimal, but other forms of reclining such as stretchers or cots are likely more available. Recliners may also be used in the case of a bed shortage.
- If additional observation is necessary, consider off-the-shelf Wi-Fi camera systems that are easy to install and can be monitored remotely.
Each patient areas in a classroom should be about 105 sf, so a typical classroom could accommodate six patients. Infection control would be “paramount,” so if carpeting is present it would need to be separated from patient care spaces or, in post-COVID-19 use, removed entirely.
Most high school HVAC systems aren’t set up to provide negative pressure used in hospitals to ward off airborne disease. But a secondary system could be set up to supplement exhaust and create negative pressurization if required.
HKS recommends converting gyms for higher patient observation areas where beds can be assembled in small groups, one bed per 190 sf. A gym could also support decentralized nursing care spaces.
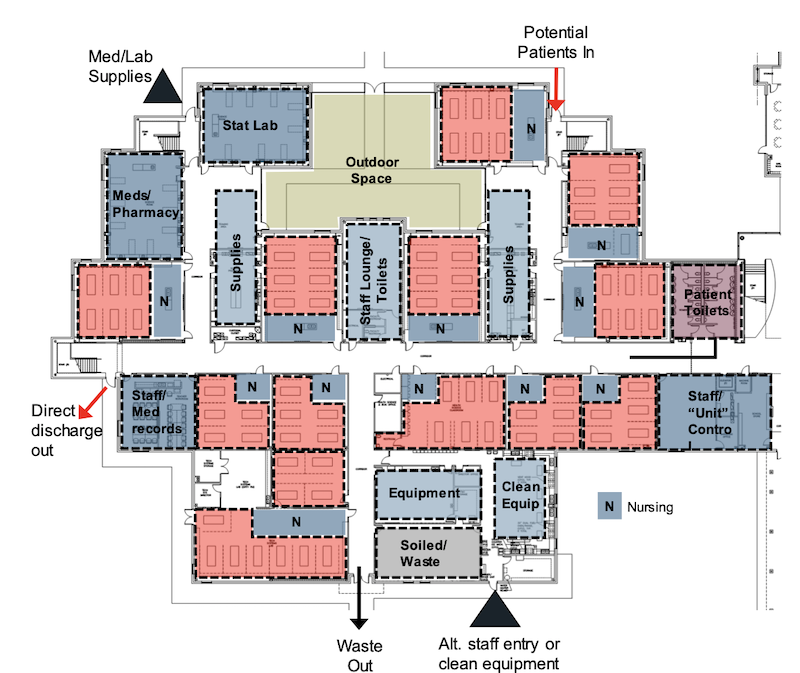
How a high school's classroom wing might accommodate 70 to 80 beds for COVID-19 patients.
There are some advantages to considering gyms for patient care conversions. For example, other support spaces such as a point-of-care testing area, stat lab, central medication storage, supply storage, waste staging and a control center could be accommodated in connected/adjacent classrooms.
On the other hand, gyms tend to have only four to five changes of locally recirculated air with three changes of outside/exhaust air per hour. Temporary ducting from central systems to the patient wards/units might be necessary, depending on the gym’s configuration.
Planners might also need to consider mobile toilets within the gymnasium/ward for closer proximity to and segregation of infectious patients. Bathing and hygiene could be accommodated at the bedside using temporary screens. Locker room showers could be used via a controlled path for ambulatory patients if the pathway to and from these rooms does not cross contaminate other traffic.
Another option within the gymnasium is to set up prefabricated patient care tents or units that can be self-contained. Some provide options for showers, toilets and sinks, if these can be connected properly to domestic water and power. Mobile electric generators should be considered to support the gymnasium function by providing additional power for medical equipment and other patient care necessities.
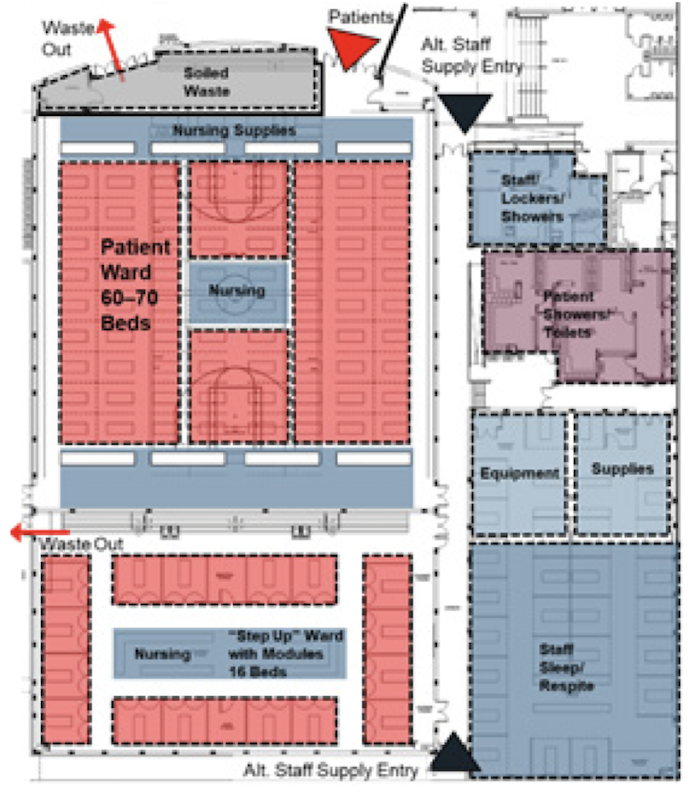
A gym converted for 70 to 80 patient beds.
HKS says that in any high school conversion, a centrally located command center is “essential” to maintaining operations and for organizational efficiency. (A library or the school’s administrative offices would be good places to put this center, HKS suggests.)
HKS’s paper offers three different conversion scenarios and how to achieve each: a high school campus that would accommodate about 400 beds, a 70- to 80-bed gym conversion, and a 70- to 80-bed classroom wing.
Related Stories
Coronavirus | Jun 30, 2020
The great reset and our new work life
As many countries begin to return to the office, it’s a chance to ask ourselves: what do we truly value?
Coronavirus | Jun 26, 2020
Infection control in buildings in the age of the coronavirus
Controlling future infection spreads could become job one for most buildings and spaces.
Coronavirus | Jun 26, 2020
ICYMI The Weekly show: The hotel sector's 'competition for cleanliness' and workplace design amid COVID-19
This week on The Weekly (June 25 episode), BD+C editors spoke with leaders from Skidmore, Owings & Merrill, Henderson Engineers, and Shawmut Design & Construction on three timely topics.
Coronavirus | Jun 23, 2020
A look back at design standard shifts: ADA vs. COVID-19
The short story is official design guidelines are slow to be developed and made into law.
Coronavirus | Jun 23, 2020
WATG designs solution for isolating without sacrificing social connectivity
The design was inspired by oriel bay windows.
Coronavirus | Jun 22, 2020
Boldt creates an innovation task force to speed up safe opening of jobsites, 14 offices
Boldt creates an innovation task force to speed up safe opening of jobsites, 14 offices
Coronavirus | Jun 19, 2020
Experts address COVID-19's impact on nursing homes and schools on The Weekly
The June 18 episode of BD+C's "The Weekly" is available for viewing on demand.
Coronavirus | Jun 18, 2020
Brown University tops off first housing building in three decades
The facility, scheduled for completion next April, will combine a residence hall with student health services.
Coronavirus | Jun 17, 2020
HOK and Germfree partner to design mobile COVID-19 testing lab
Access to quick, reliable, and repeated testing has been one of the greatest challenges for businesses, institutions and individuals during the COVID-19 crisis.
Coronavirus | Jun 17, 2020
Guiding changes in the workplace: Past, present, and future
Since the COVID-19 pandemic, many companies are managing sudden change as they assess the impact on workplace design and how people use spaces.