Looking at trends and predictions from the beginning of 2013, many anticipated that it would be a transformational year as healthcare organizations evolved to confront the challenges of a changing marketplace. As the year draws to a close and we look to the future, despite the lack of clarity regarding many elements of healthcare reform, there are several core tenets that will likely continue to drive transition within our industry.
While each of these trends is widely acknowledged and publicized, their pervasive impact on healthcare real estate warrants further examination. Healthcare providers will be challenged to provide higher quality care to an expanded patient base at a significantly lower overall cost. To achieve these objectives and thrive in the marketplace of the future, many healthcare organizations will be required to transition and transform their portfolio of real estate assets, as well as the manner in which those assets are planned, financed, constructed and managed.
1. INSURANCE EXPANSION AND REFORM
Expanded Coverage for All?
Until very recently, prevailing expectations held that the Affordable Care Act would result in a net increase in the number of insured Americans by as many as 30 million individuals. However, the highly publicized shortcomings of government sponsored insurance enrollment portals, the relative lack of interest in enrollment among younger age cohorts and the increasing number of individuals receiving coverage cancellation notices in the past two months may actually result in a short term decrease in the total insured population.
Financial Incentives - Focus on Patient Outcomes
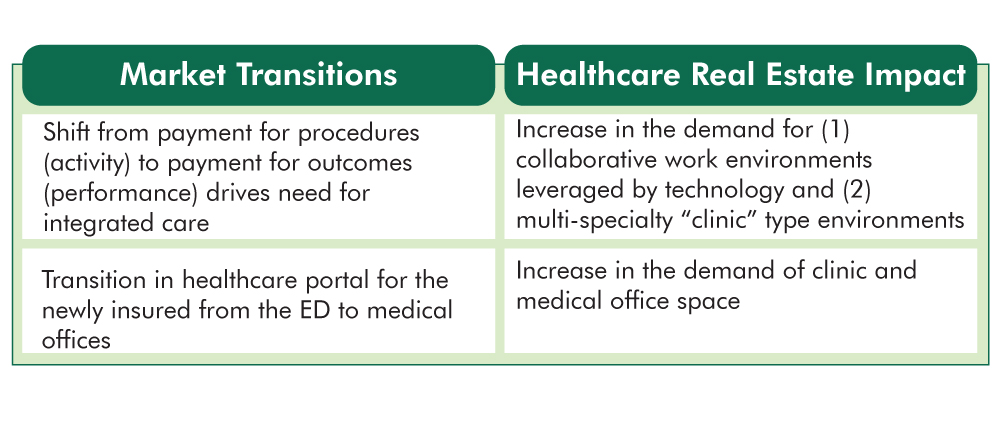
Providers have traditionally been compensated for episodes of care. There has been little financial incentive to coordinate care between physicians and many procedures are criticized as contributing little to patient outcomes. This reimbursement environment is commonly criticized as a primary driver in the escalation of healthcare expenditures in this nation.
A central objective of the Affordable Care Act is to transition to a Value Based Reimbursement environment in which “bundled payments” are made to coordinated teams of care providers and are based on patient outcomes rather than the number of procedures performed. There will be little to no reimbursement for patient readmissions. This seismic shift will mandate that high quality patient outcomes are achieved consistently in the most coordinated and efficient manner possible.
Responding to Insurance Expansion and Reform – The Role of Healthcare Real Estate: So, how does real estate enter the discussion regarding insurance and financial incentives? To achieve the objective of delivering best in class patient outcomes in a consistent manner at the lowest possible cost, providers will benefit significantly from standardizing best practices across their organizations. As “form follows function”, healthcare real estate portfolios must be comprised of replicable care environments. It is difficult to expect consistent patient outcomes unless the very environment in which that care is delivered is also consistent.
2. TRANSFORMING THE ORGANIZATIONAL MODEL OF CARE
Here Today....There Tomorrow
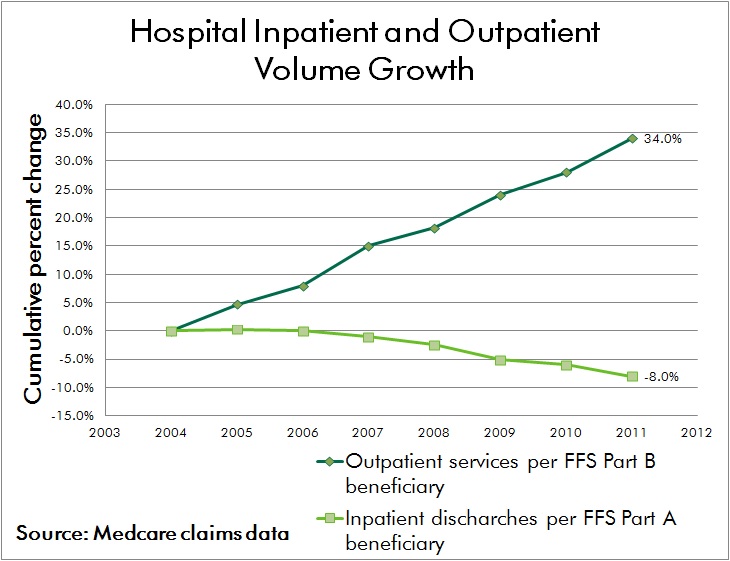
Advances in medical technology have driven a shift in procedural volume to the outpatient environment for decades. With the added imperative to provide care in the lowest cost responsible setting, this trend is expected to continue. Advances in technology will not only enable a continued shift from inpatient to outpatient procedures, but it’s highly likely that certain elements of care currently provided in outpatient and medical office environments can be achieved through remote monitoring and electronic communication while patients remain at home or work.
Organizing for Success
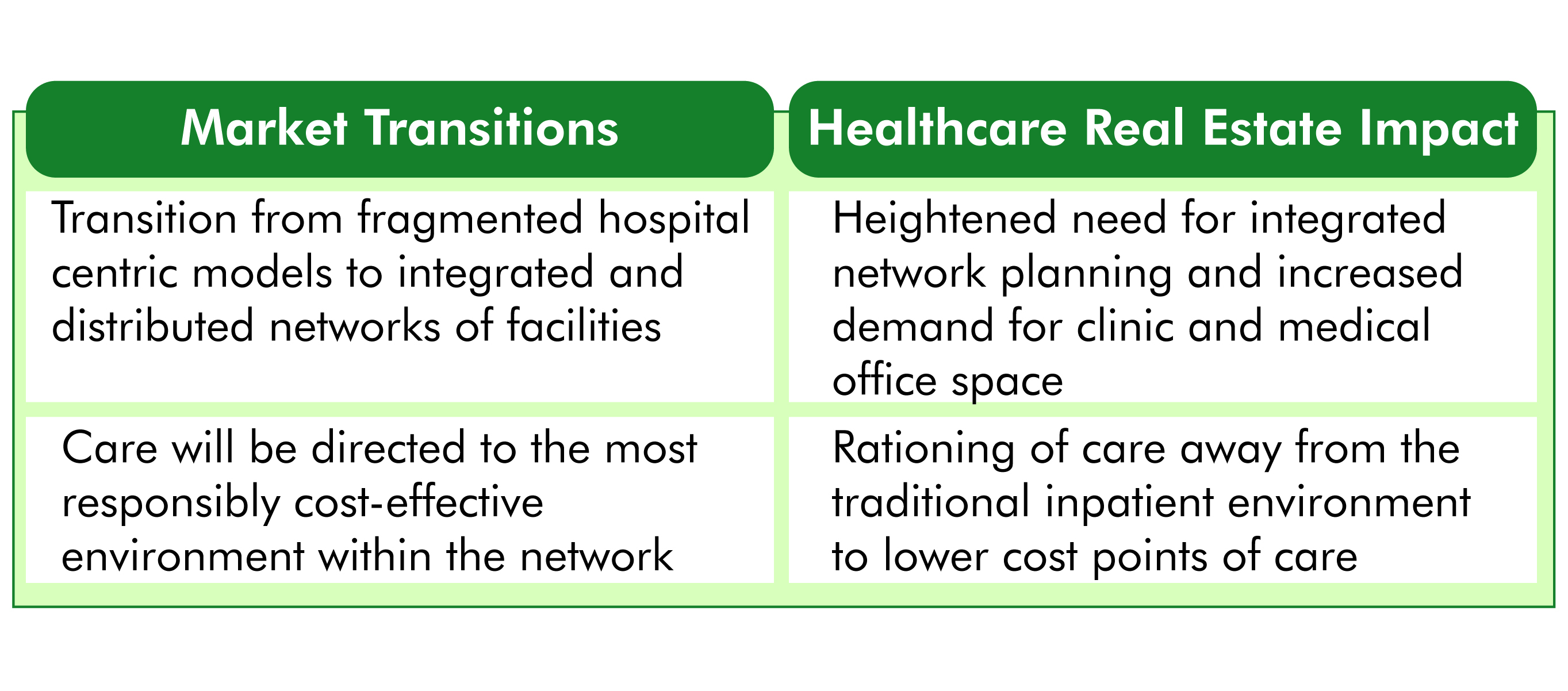
While the physical environment of care continues to shift, the organizational structure of healthcare providers must keep pace as well. The hospital centric model of the past has already given way to a hub and spoke network of care in most markets, where outpatient centers provide convenient and accessible care to patients and refer volumes to affiliated inpatient facilities.
The prevailing hub and spoke network will give way to a distributed model of care that is physically dispersed yet highly integrated. Electronic medical records and advances in medical information technology will allow seamless handoffs between care providers, many of whom will be geographically dispersed across the network. Primary care and internal medicine specialists will coordinate care regimens, a patient centric concept known as the “medical home.”
Responding to Organizational Transformation – The Role of Healthcare Real Estate: Reflecting the significant capital investment in acute care facilities and traditional medical office environments that currently resides on providers’ balance sheets, the transition of healthcare real estate portfolios to nimble, distributed networks of care will be a long term process. Given the lengthy cycle of major facility planning and development schedules, it's imperative that providers initiate coordinated market and facility planning efforts today in order to begin their journey of transformation.
3. MARGIN COMPRESSION
The Future Ain’t What it Used to Be
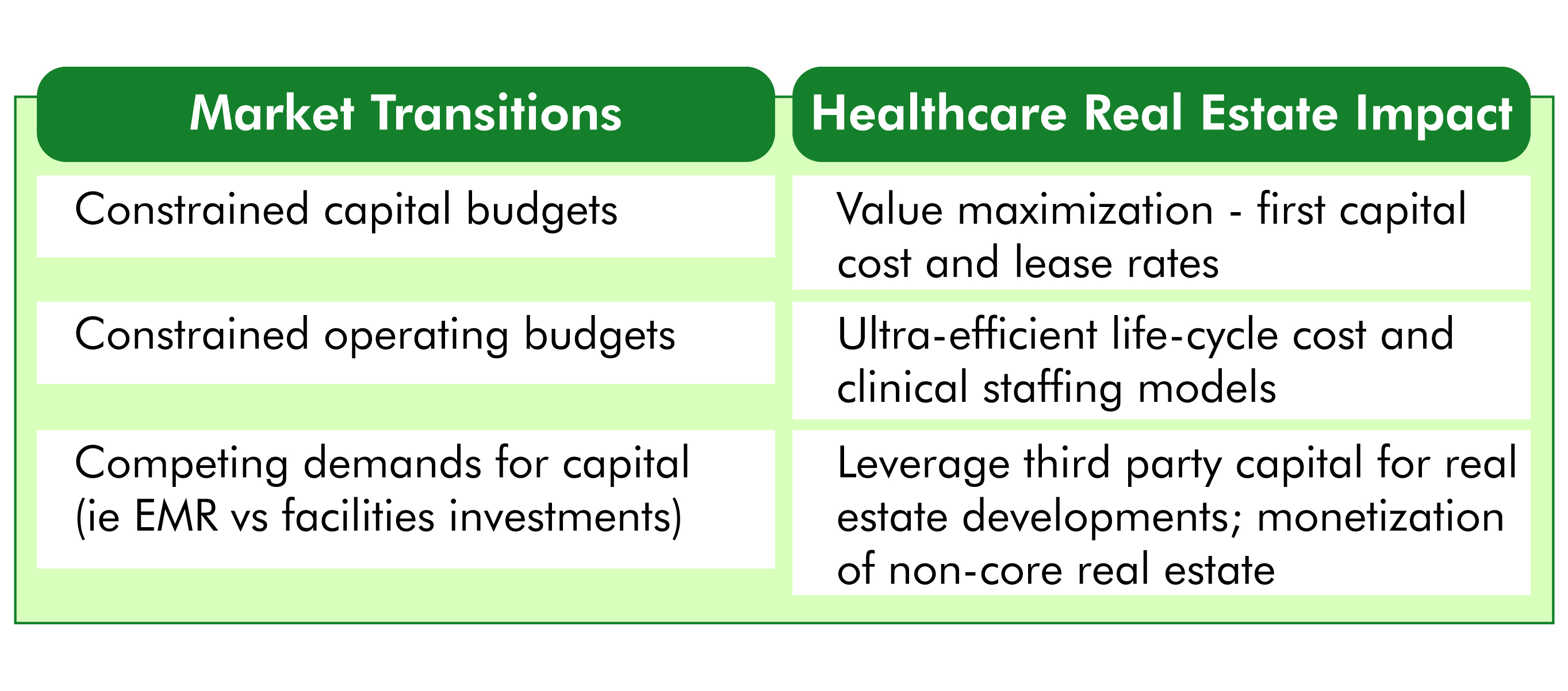
The seismic shifts in healthcare finance being driven by insurance reform threaten the long term viability of many healthcare providers who have traditionally operated near breakeven. According to Moody's Investors Service, nonprofit hospitals had a strong balance sheer in fiscal year 2012 but profitability metrics were down compared with FY 2011. For the first time since FY 2008, Moody's found that growth in expenses outpaced revenue growth in nonprofit hospitals and health systems. Even a modest shift in revenue outlook for these organizations may constitute the difference between operating in the black or confronting financial loss.
While a substantial portion of the nation’s hospitals and health systems are non-profit institutions, there is common recognition that erosion of financial performance will compromise the ability to provide philanthropic and charity care. “No margin – No mission.” Few expect brighter prospects for revenue; therefore, organizational survival will depend on the ability to decrease expenditures without compromising care.
Competing Demands for Scarce Capital
Despite concern regarding future operating margins, the demand for capital investment is greater than ever. Conversion to electronic medical records is an enormously expensive undertaking, often running into the hundreds of millions of dollars for large health systems. Mergers, acquisitions and affiliations among providers also demand organizational focus and capital.
Responding to Margin Compression – The Role of Healthcare Real Estate: Real estate assets often constitute the single greatest balance sheet asset for healthcare providers and real estate related expenses are typically exceeded only by the cost of labor on providers’ income statements. To meet the imperative of cost reduction, in the most general terms, healthcare real estate must be developed and operated in a more cost effective manner. Facility layouts also have an integral impact on the efficiency of patient care delivery processes; and therefore play a key role in reducing labor expense without compromising quality of care.
4. INDUSTRY CONSOLIDATION
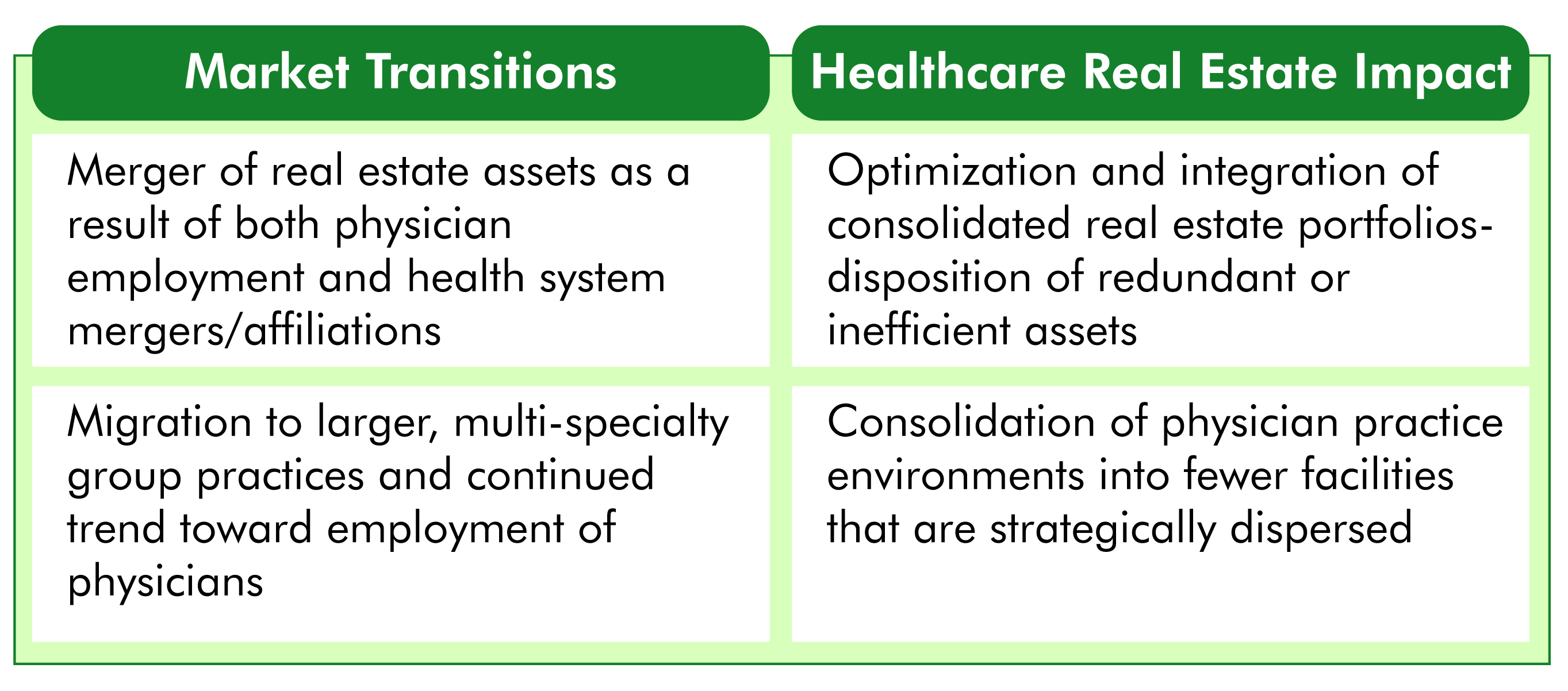
One of the most significant byproducts of insurance reform and financial pressures faced by healthcare providers has been an unprecedented wave of industry consolidation. Many independent hospitals and small health systems are not sufficiently capitalized to effectively reinvest and reinvent themselves. Similar challenges are faced by physicians operating in small group practices as they struggle to cover traditional costs such as malpractice insurance, as well as the added burden of conversion to electronic medical records.
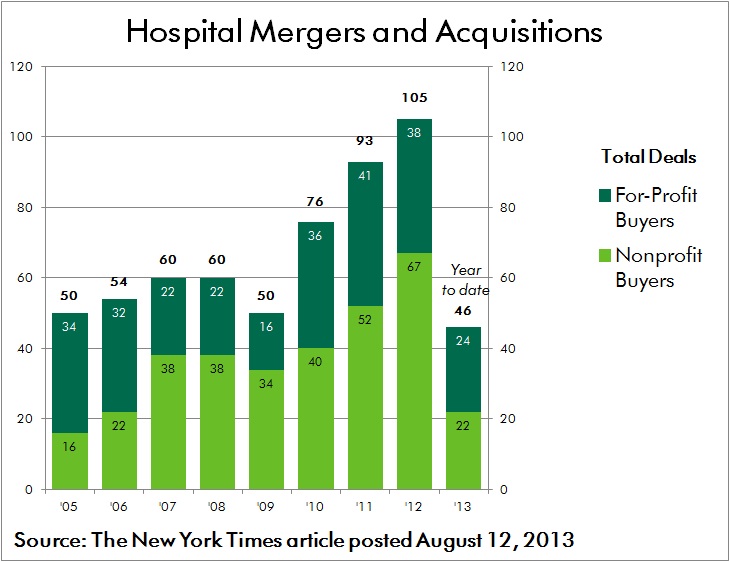
Coupled with the prospect of “bundled payment” reimbursements, these forces are driving consolidation in order to allow providers to better coordinate care and to spread costly investments across a larger operating platform. According to an Irving Levin report, healthcare mergers and acquisitions activity during the third quarter this year soared 16 percent over the second quarter of 2013. There were 267 deals announced, which is 20 percent more than the third quarter last year. Many of these alliances break from the traditional mold, including the acquisition of physician practices by insurance providers.
Responding to Consolidation – The Role of Healthcare Real Estate: As health systems, hospitals and physician groups merge and affiliate, the resulting portfolio of assets is often poorly positioned to serve the organization’s needs in an efficient manner. Fragmented networks of leased and owned facilities are located in close proximity to each other. Multiple systems and protocols are used to manage the development and operation of assets. Legacy policies and procedures are not synchronized.
To meet the challenges of coordinated care and cost reduction, a transition plan must be enacted through which optimal facility network distribution and co-location of care providers is achieved. In many cases this will result in the consolidation of redundant and inefficient facilities, while in other cases there will be a need to develop facilities in new markets in order to effectively achieve population health management goals. Migrating to a common, best in class platform for managing consolidated portfolios of facilities often requires investment in both training and new technology.
CONCLUSION
As the pace of transformative change within the industry accelerates, healthcare leaders must heed the call to act decisively in order to position their organizations for survival and success. Effective planning, development and operation of healthcare real estate assets will be a critical element in ensuring that best in class, patient centered care is delivered consistently and cost effectively. As margins are compressed and care is increasingly distributed across broader provider networks, the integration of strategic, financial and facility initiatives is more critical than ever.
Within every challenge lies opportunity. Best wishes to all in capitalizing on those opportunities in the year ahead.
Related Stories
Sustainable Design and Construction | Oct 10, 2024
Northglenn, a Denver suburb, opens a net zero, all-electric city hall with a mass timber structure
Northglenn, Colo., a Denver suburb, has opened the new Northglenn City Hall—a net zero, fully electric building with a mass timber structure. The 32,600-sf, $33.7 million building houses 60 city staffers. Designed by Anderson Mason Dale Architects, Northglenn City Hall is set to become the first municipal building in Colorado, and one of the first in the country, to achieve the Core certification: a green building rating system overseen by the International Living Future Institute.
3D Printing | Oct 9, 2024
3D-printed construction milestones take shape in Tennessee and Texas
Two notable 3D-printed projects mark milestones in the new construction technique of “printing” structures with specialized concrete. In Athens, Tennessee, Walmart hired Alquist 3D to build a 20-foot-high store expansion, one of the largest freestanding 3D-printed commercial concrete structures in the U.S. In Marfa, Texas, the world’s first 3D-printed hotel is under construction at an existing hotel and campground site.
University Buildings | Oct 9, 2024
Des Moines University Medicine and Health Sciences opens a new 88-acre campus
Des Moines University Medicine and Health Sciences has opened a new campus spanning 88 acres, over three times larger than its previous location. Designed by RDG Planning & Design and built by Turner Construction, the $260 million campus features technology-rich, flexible educational spaces that promote innovative teaching methods, expand research activity, and enhance clinical services. The campus includes four buildings connected with elevated pathways and totaling 382,000 sf.
Student Housing | Oct 9, 2024
University of Maryland begins work on $148 million graduate student housing development
The University of Maryland, in partnership with Campus Apartments and Mosaic Development Partners, has broken ground on a $148.75 million graduate student housing project on the university’s flagship College Park campus. The project will add 741 beds in 465 fully furnished apartments.
AEC Tech Innovation | Oct 8, 2024
New ABC technology report examines how AI can enhance efficiency, innovation
The latest annual technology report from Associated Builders and Contractors delves into how artificial intelligence can enhance efficiency and innovation in the construction sector. The report includes a resource guide, a case study, insight papers, and an essay concerning applied uses for AI planning, development, and execution.
Healthcare Facilities | Oct 8, 2024
Herzog & de Meuron completes Switzerland’s largest children’s hospital
The new University Children’s Hospital Zurich features 114 rooftop patient rooms designed like wooden cottages with their own roofs. The project also includes a research and teaching facility.
Mixed-Use | Oct 7, 2024
New mixed-use tower by Studio Gang completes first phase of San Francisco waterfront redevelopment
Construction was recently completed on Verde, a new mixed-use tower along the San Francisco waterfront, marking the end of the first phase of the Mission Rock development. Verde is the fourth and final building of phase one of the 28-acre project that will be constructed in several phases guided by design principles developed by a design cohort led by Studio Gang.
Brick and Masonry | Oct 7, 2024
A journey through masonry reclad litigation
This blog post by Walter P Moore's Mallory Buckley, RRO, PE, BECxP + CxA+BE, and Bob Hancock, MBA, JD, of Munsch Hardt Kopf & Harr PC, explains the importance of documentation, correspondence between parties, and supporting the claims for a Plaintiff-party, while facilitating continuous use of the facility, on construction litigation projects.
University Buildings | Oct 4, 2024
Renovations are raising higher education campuses to modern standards
AEC higher ed Giants report working on a variety of building types, from performing arts centers and libraries to business schools. Hybrid learning is seemingly here to stay. And where possible, these projects address wellness and mental health concerns.
Laboratories | Oct 2, 2024
Trends in scientific research environments: Q&A with Flad's Matt McCord
As part of an ongoing series, Matt McCord, AIA, NCARB, LEED AP BD+C, Associate Principal with Flad Architects, discusses the future of the scientific workplace.