Healthcare consumers are just as likely to factor in convenience as they do cost when deciding where to seek care and from whom, according to a new survey of 4,037 American adults about their attitudes and preferences as patients.
The survey, conducted from April 19-28 by JLL, in many ways confirms the obvious: that older generations seek preventive care more often than younger generations; that insurance coverage is a primary driver for choosing a provider or hospital; and that the quality of service affects the patient experience.
Nearly eight of 10 of the survey’s respondents had received at least one type of non-dental care in the last year. Women, who accounted for 51% of the survey’s respondents, are more likely to receive care overall, but men are more likely to receive emergency care.
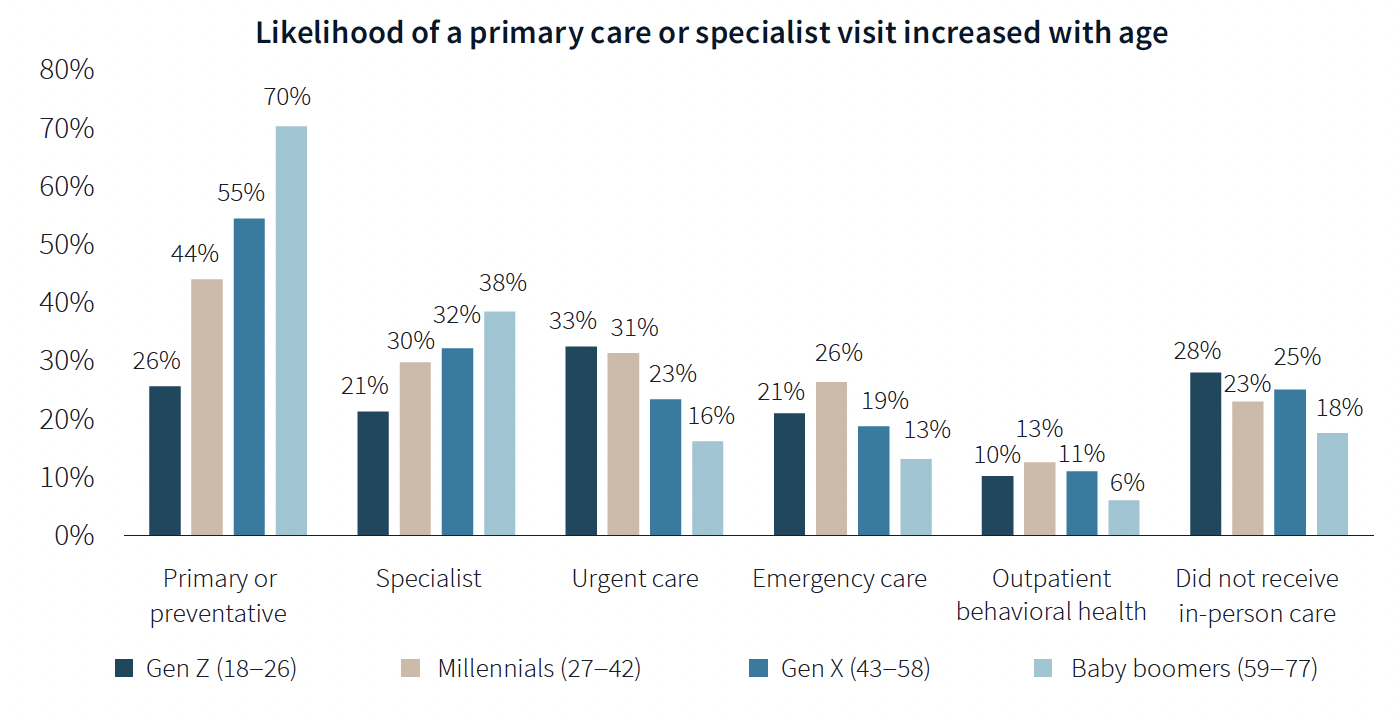
The likelihood of a primary care or specialist visit increases with age: 80% of adults 65 years or older have two or more chronic conditions that require continuous care. More than 70% of Baby Boomers (who accounted for 29% of the survey’s respondents) had received primary or preventive care within the last year, compared to only 26% of Generation Z.
Younger generations are more reactive than preventive in their healthcare decisions, borne out by the survey’s finding that Millennials and Gen Zs (43% of the survey's respondents) are more likely to receive urgent care, emergency care, and outpatient behavioral healthcare than older adults.
Proximity to patients counts
When care is urgently needed, “decision factors are simplified,” the survey states, and location and proximity of care are ranked higher as decision-making factors. But even outside of emergencies, convenience ranks high among factors for patients seeking care.
There’s no denying that cost is always in the background of any healthcare decision. “Accept my insurance” was the most common factor for choosing a provider among the survey’s respondents. (82% of participants has private insurance, and 81% has public insurance.)
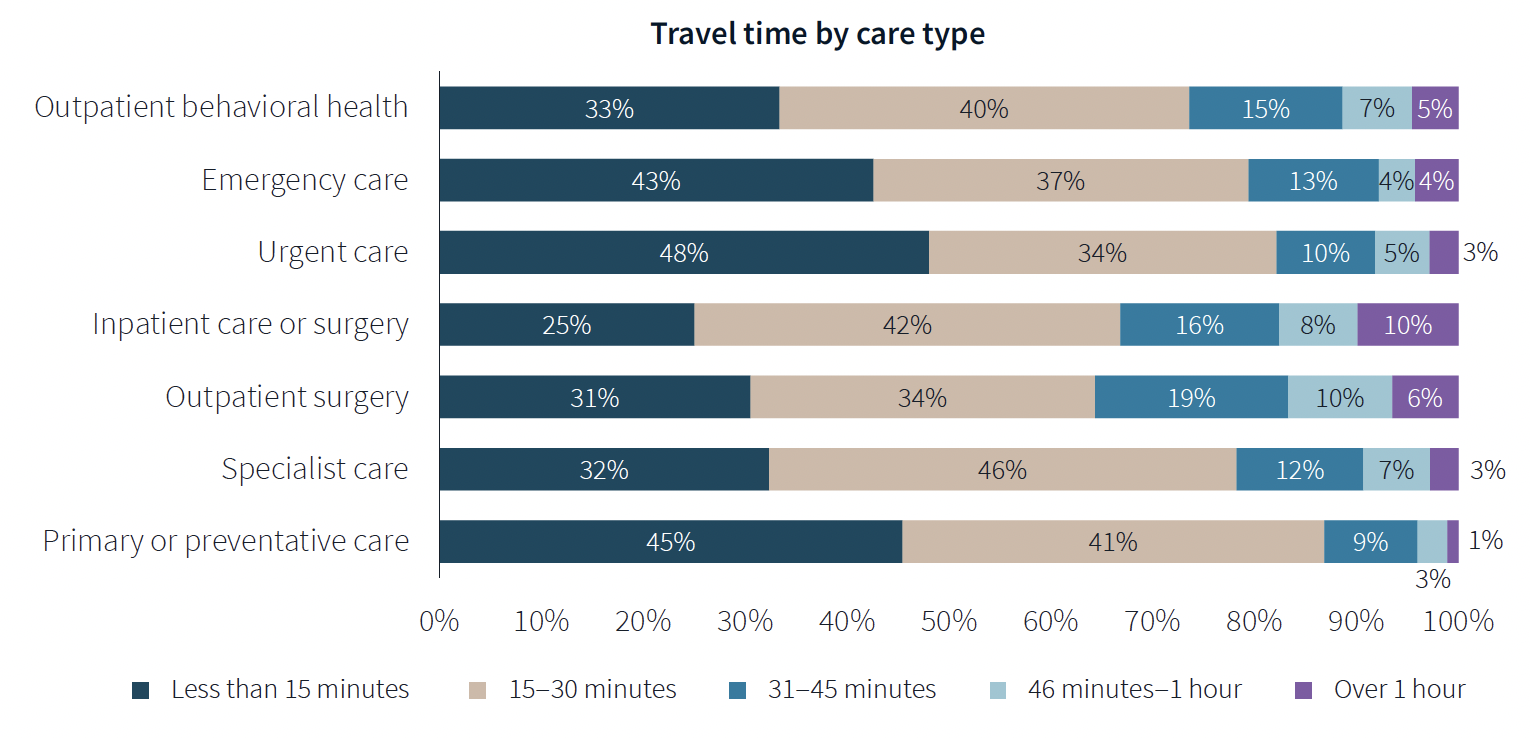
Two-fifths of respondents said they travel less than 15 minutes to receive care, and nearly eight of 10 respondents travel less than 30 minutes. Among those with appointments in standalone medical offices, 85% ranked location as convenience, which the survey suggested indicates the advantages of a dispersed location strategy.
“A strong location strategy can improve reach for health systems and physician practices and potentially improve care outcomes,” JLL writes. “But there is a balance between convenience and cost—health systems need to balance the benefits of being close to their target population with the cost of a new facility or doctors’ time in transit from a local clinic to the hospital.”
Convenience is also key both in location and in being able to navigate to care. Patients want to get to care quickly and get on with their day. Ease of parking and ability to navigate the facility also affected a facility’s net positive score in the survey.
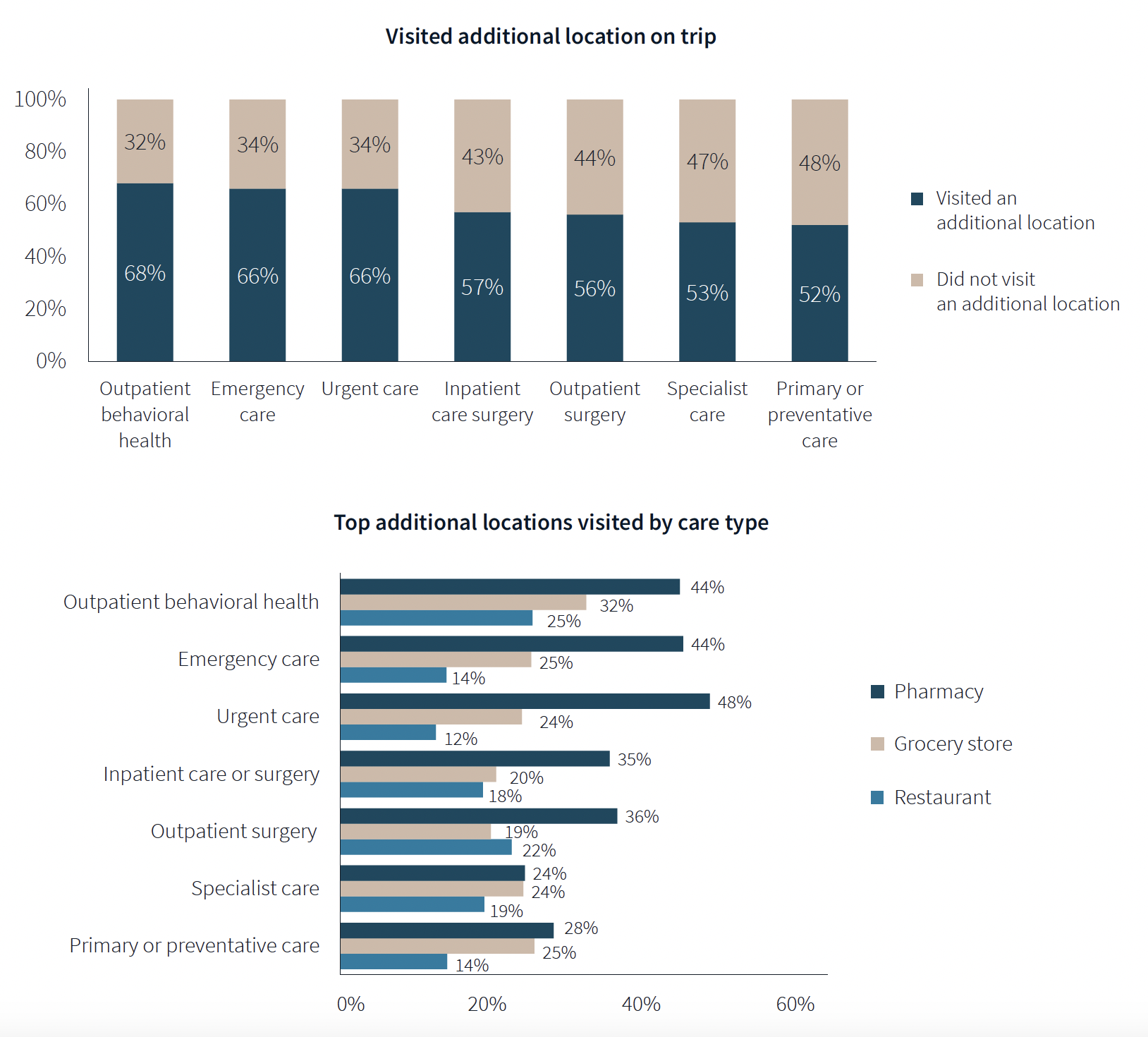
One of the survey’s more revealing findings is that nearly three-fifths of respondents—58%—went to another location—such as a pharmacy, or an urgent clinic—as part of their trip for healthcare.
Word of mouth often defines quality of care
Patients seem to be open to diverse care choices. For example, 29% said they have visited a retail clinic, such as a CVS, and would do so again. Gen Z and Millennials are more likely to frequent retail clinics for their convenient appointment schedules and shorter wait times.
More than two-fifths of respondents—42%—had a telehealth appointment within the last year, which was slightly down from the 45% in JLL’s 2022 survey. This year’s poll also found that 29% of telehealth appointments led to an in-person visit.
More than 40% of respondents ranked “reputation of quality” among the top five factors for choosing care. But where they get their impressions about quality varies.
Referrals play a larger role in specialist, outpatient surgery and inpatient care. Recommendations from friends ranked most highly for behavioral health, given the personal nature of such care, and was ranked in the top five by 31% of respondents. Younger patients, who “have yet to develop brand loyalty,” according to the survey, are more likely to rely on word-of-mouth recommendations than older patients for whom hospital systems’ reps matter more.
Outpatient surgery and primary care ranked highest for provider satisfaction; emergency care ranked lowest. Participants ranked their experiences on 12 aspects of care, and the biggest gap between “promoters” and “detractors” was for the service level of providers. Primary care had the highest net provider score, with 86% of respondents ranking its care as “attentive.”
Some amenities draw patients
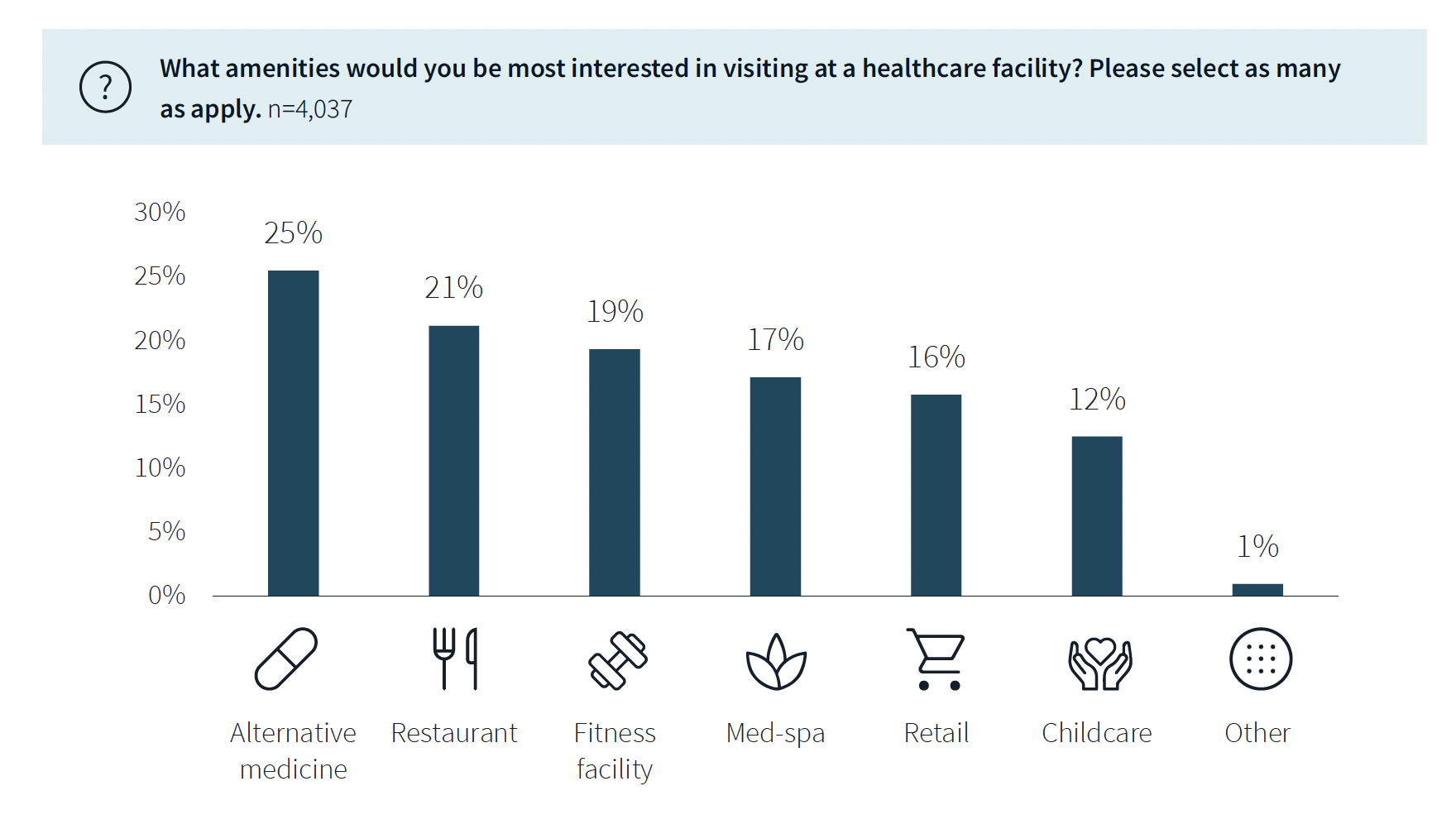
While not a decision-making factor, amenities do attract some patients. Among the survey’s respondents, 63% said they would be interested in visiting a healthcare facility with an additional amenity, such as alternative medicine, a restaurant, fitness center, or spa. (This inclination was more evident among younger respondents.)
The overall quality of facilities, including the comfort of their waiting rooms, can impact a patient’s choice, especially for inpatient, urgent, and emergency care. The survey also found that urban locations have lower favorability rankings for their facilities, signaling room for improvement. (Just under half—48%—of respondents live in the suburbs.)
Related Stories
| Jan 31, 2011
CISCA releases White Paper on Acoustics in Healthcare Environments
The Ceilings & Interior Systems Construction Association (CISCA) has released an extensive white paper “Acoustics in Healthcare Environments” for architects, interior designers, and other design professionals who work to improve healthcare settings for all users. This white paper serves as a comprehensive introduction to the acoustical issues commonly confronted on healthcare projects and howbest to address those.
| Jan 27, 2011
Perkins Eastman's report on senior housing signals a changing market
Top international design and architecture firm Perkins Eastman is pleased to announce that the Perkins Eastman Research Collaborative recently completed the “Design for Aging Review 10 Insights and Innovations: The State of Senior Housing” study for the American Institute of Architects (AIA). The results of the comprehensive study reflect the changing demands and emerging concepts that are re-shaping today’s senior living industry.
| Jan 21, 2011
Harlem facility combines social services with retail, office space
Harlem is one of the first neighborhoods in New York City to combine retail with assisted living. The six-story, 50,000-sf building provides assisted living for residents with disabilities and a nonprofit group offering services to minority groups, plus retail and office space.
| Jan 21, 2011
Research center built for interdisciplinary cooperation
The Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital, in Houston, the first basic research institute for childhood neurological diseases, is a 13-story twisting tower in the center of the hospital campus.
| Jan 19, 2011
Biomedical research center in Texas to foster scientific collaboration
The new Health and Biomedical Sciences Center at the University of Houston will facilitate interaction between scientists in a 167,000-sf, six-story research facility. The center will bring together researchers from many of the school’s departments to collaborate on interdisciplinary projects. The facility also will feature an ambulatory surgery center for the College of Optometry, the first of its kind for an optometry school. Boston-based firms Shepley Bulfinch and Bailey Architects designed the project.
| Jan 19, 2011
New Fort Hood hospital will replace aging medical center
The Army Corps of Engineers selected London-based Balfour Beatty and St. Louis-based McCarthy to provide design-build services for the Fort Hood Replacement Hospital in Texas, a $503 million, 944,000-sf complex partially funded by the American Recovery and Reinvestment Act. The firm plans to use BIM for the project, which will include outpatient clinics, an ambulance garage, a central utility plant, and three parking structures. Texas firms HKS Architects and Wingler & Sharp will participate as design partners. The project seeks LEED Gold.
| Jan 10, 2011
Michael J. Alter, president of The Alter Group: ‘There’s a significant pent-up demand for projects’
Michael J. Alter, president of The Alter Group, a national corporate real estate development firm headquartered in Skokie, Ill., on the growth of urban centers, project financing, and what clients are saying about sustainability.
| Dec 17, 2010
ARRA-funded Navy hospital aims for LEED Gold
The team of Clark/McCarthy, HKS Architects, and Wingler & Sharp are collaborating on the design of a new naval hospital at Camp Pendleton in Southern California. The $451 million project is the largest so far awarded by the U.S. Navy under the American Recovery and Reinvestment Act. The 500,000-sf, 67-bed hospital, to be located on a 70-acre site, will include facilities for emergency and primary care, specialty care clinics, surgery, and intensive care. The Building Team is targeting LEED Gold.
| Dec 17, 2010
Arizona outpatient cancer center to light a ‘lantern of hope’
Construction of the Banner MD Anderson Cancer Center in Gilbert, Ariz., is under way. Located on the Banner Gateway Medical Center campus near Phoenix, the three-story, 131,000-sf outpatient facility will house radiation oncology, outpatient imaging, multi-specialty clinics, infusion therapy, and various support services. Cannon Design incorporated a signature architectural feature called the “lantern of hope” for the $90 million facility.
| Oct 18, 2010
World’s first zero-carbon city on track in Abu Dhabi
Masdar City, the world’s only zero-carbon city, is on track to be built in Abu Dhabi, with completion expected as early as 2020. Foster + Partners developed the $22 billion city’s master plan, with Adrian Smith + Gordon Gill Architecture, Aedas, and Lava Architects designing buildings for the project’s first phase, which is on track to be ready for occupancy by 2015.














