Healthcare consumers are just as likely to factor in convenience as they do cost when deciding where to seek care and from whom, according to a new survey of 4,037 American adults about their attitudes and preferences as patients.
The survey, conducted from April 19-28 by JLL, in many ways confirms the obvious: that older generations seek preventive care more often than younger generations; that insurance coverage is a primary driver for choosing a provider or hospital; and that the quality of service affects the patient experience.
Nearly eight of 10 of the survey’s respondents had received at least one type of non-dental care in the last year. Women, who accounted for 51% of the survey’s respondents, are more likely to receive care overall, but men are more likely to receive emergency care.
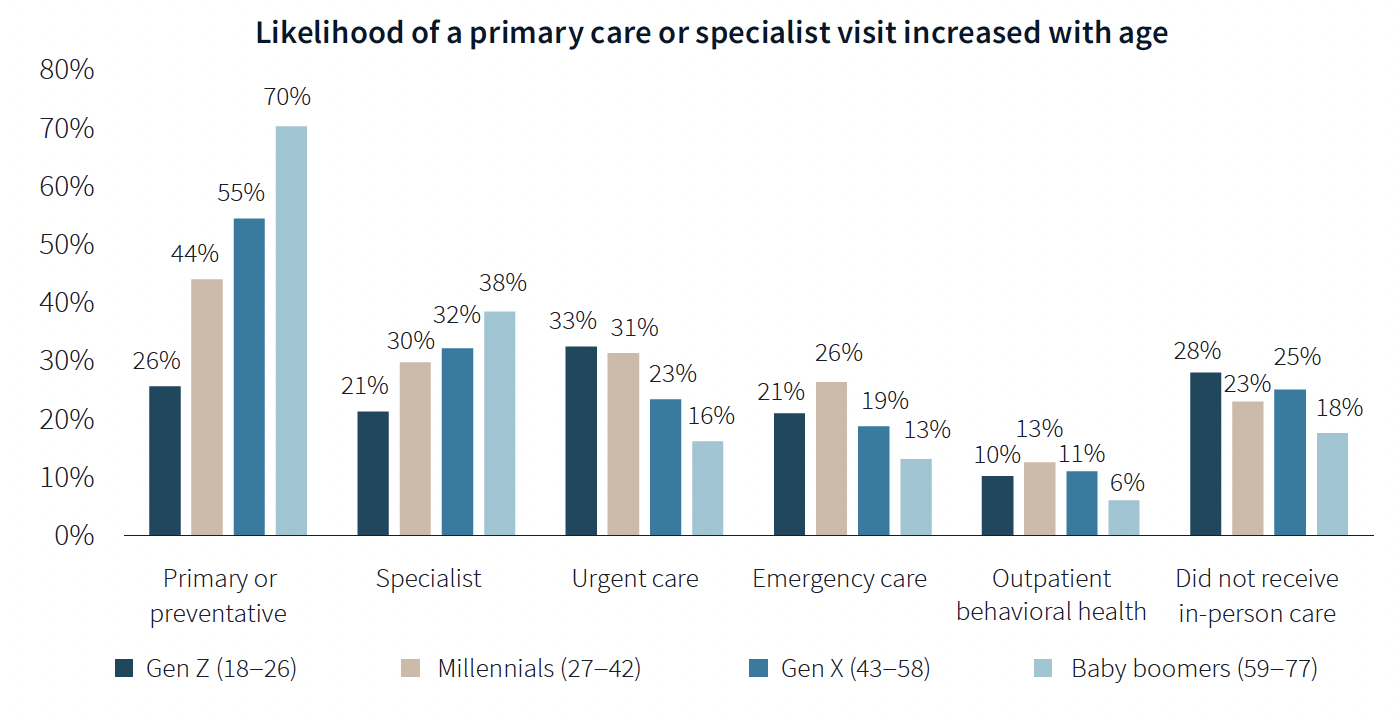
The likelihood of a primary care or specialist visit increases with age: 80% of adults 65 years or older have two or more chronic conditions that require continuous care. More than 70% of Baby Boomers (who accounted for 29% of the survey’s respondents) had received primary or preventive care within the last year, compared to only 26% of Generation Z.
Younger generations are more reactive than preventive in their healthcare decisions, borne out by the survey’s finding that Millennials and Gen Zs (43% of the survey's respondents) are more likely to receive urgent care, emergency care, and outpatient behavioral healthcare than older adults.
Proximity to patients counts
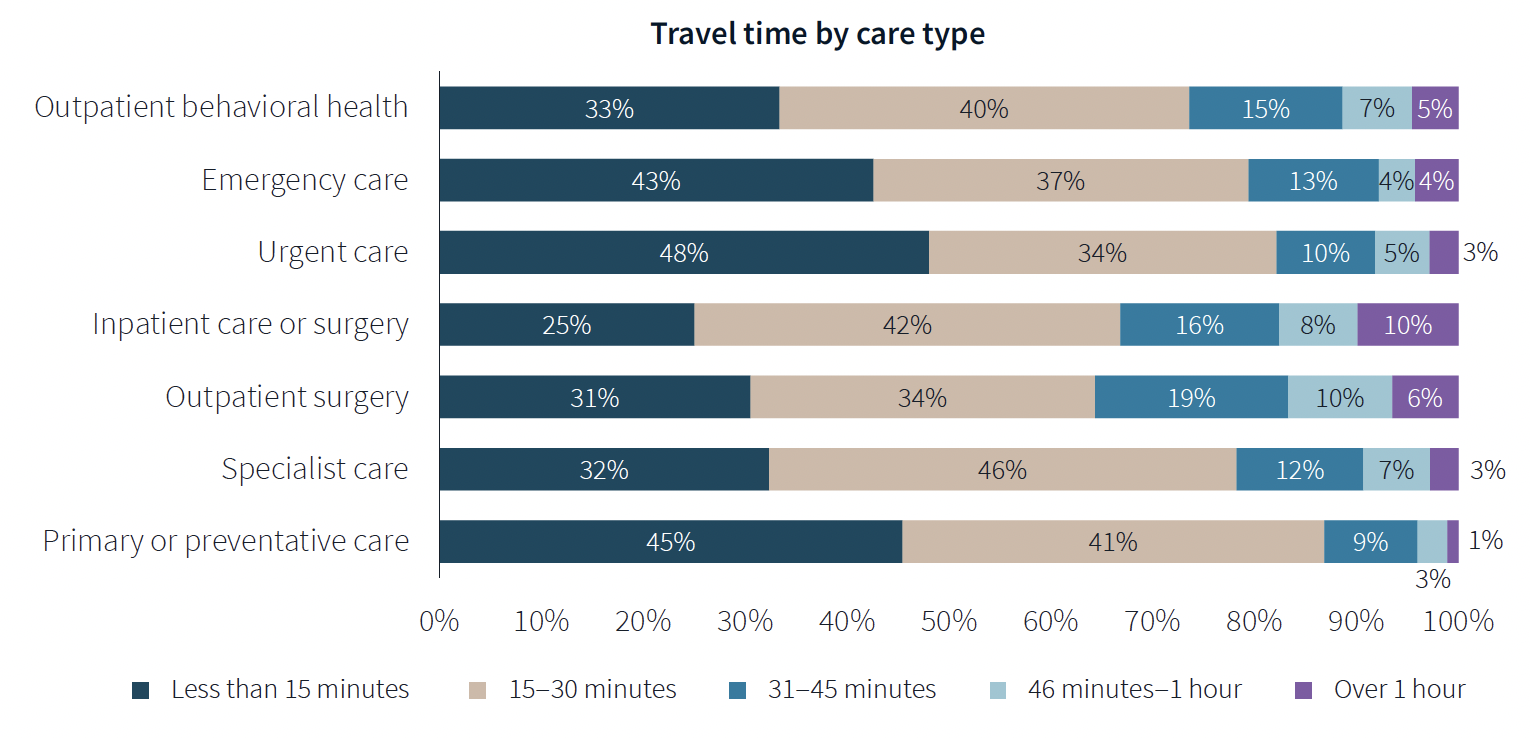
When care is urgently needed, “decision factors are simplified,” the survey states, and location and proximity of care are ranked higher as decision-making factors. But even outside of emergencies, convenience ranks high among factors for patients seeking care.
There’s no denying that cost is always in the background of any healthcare decision. “Accept my insurance” was the most common factor for choosing a provider among the survey’s respondents. (82% of participants has private insurance, and 81% has public insurance.)
Two-fifths of respondents said they travel less than 15 minutes to receive care, and nearly eight of 10 respondents travel less than 30 minutes. Among those with appointments in standalone medical offices, 85% ranked location as convenience, which the survey suggested indicates the advantages of a dispersed location strategy.
“A strong location strategy can improve reach for health systems and physician practices and potentially improve care outcomes,” JLL writes. “But there is a balance between convenience and cost—health systems need to balance the benefits of being close to their target population with the cost of a new facility or doctors’ time in transit from a local clinic to the hospital.”
Convenience is also key both in location and in being able to navigate to care. Patients want to get to care quickly and get on with their day. Ease of parking and ability to navigate the facility also affected a facility’s net positive score in the survey.
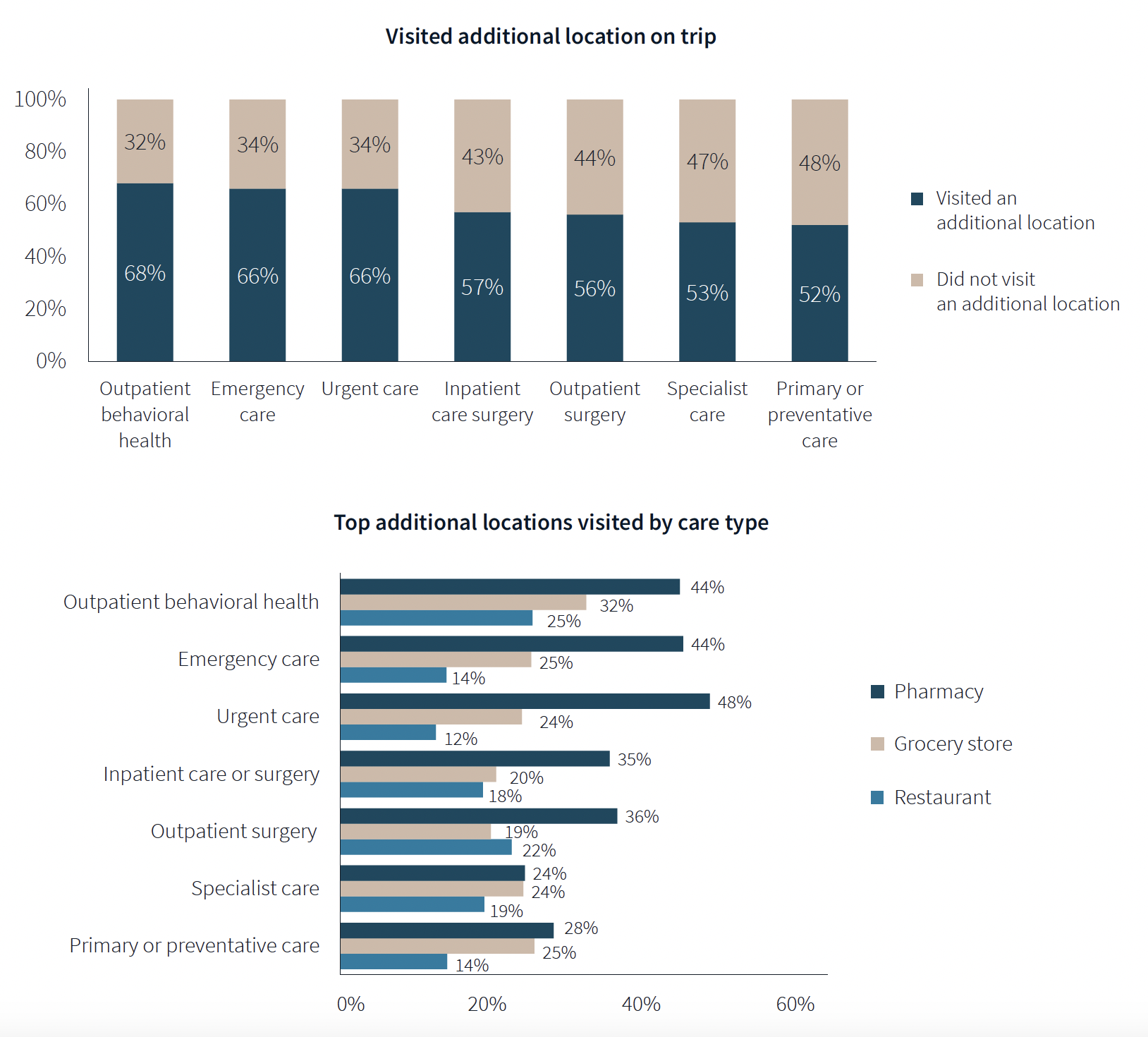
One of the survey’s more revealing findings is that nearly three-fifths of respondents—58%—went to another location—such as a pharmacy, or an urgent clinic—as part of their trip for healthcare.
Word of mouth often defines quality of care
Patients seem to be open to diverse care choices. For example, 29% said they have visited a retail clinic, such as a CVS, and would do so again. Gen Z and Millennials are more likely to frequent retail clinics for their convenient appointment schedules and shorter wait times.
More than two-fifths of respondents—42%—had a telehealth appointment within the last year, which was slightly down from the 45% in JLL’s 2022 survey. This year’s poll also found that 29% of telehealth appointments led to an in-person visit.
More than 40% of respondents ranked “reputation of quality” among the top five factors for choosing care. But where they get their impressions about quality varies.
Referrals play a larger role in specialist, outpatient surgery and inpatient care. Recommendations from friends ranked most highly for behavioral health, given the personal nature of such care, and was ranked in the top five by 31% of respondents. Younger patients, who “have yet to develop brand loyalty,” according to the survey, are more likely to rely on word-of-mouth recommendations than older patients for whom hospital systems’ reps matter more.
Outpatient surgery and primary care ranked highest for provider satisfaction; emergency care ranked lowest. Participants ranked their experiences on 12 aspects of care, and the biggest gap between “promoters” and “detractors” was for the service level of providers. Primary care had the highest net provider score, with 86% of respondents ranking its care as “attentive.”
Some amenities draw patients
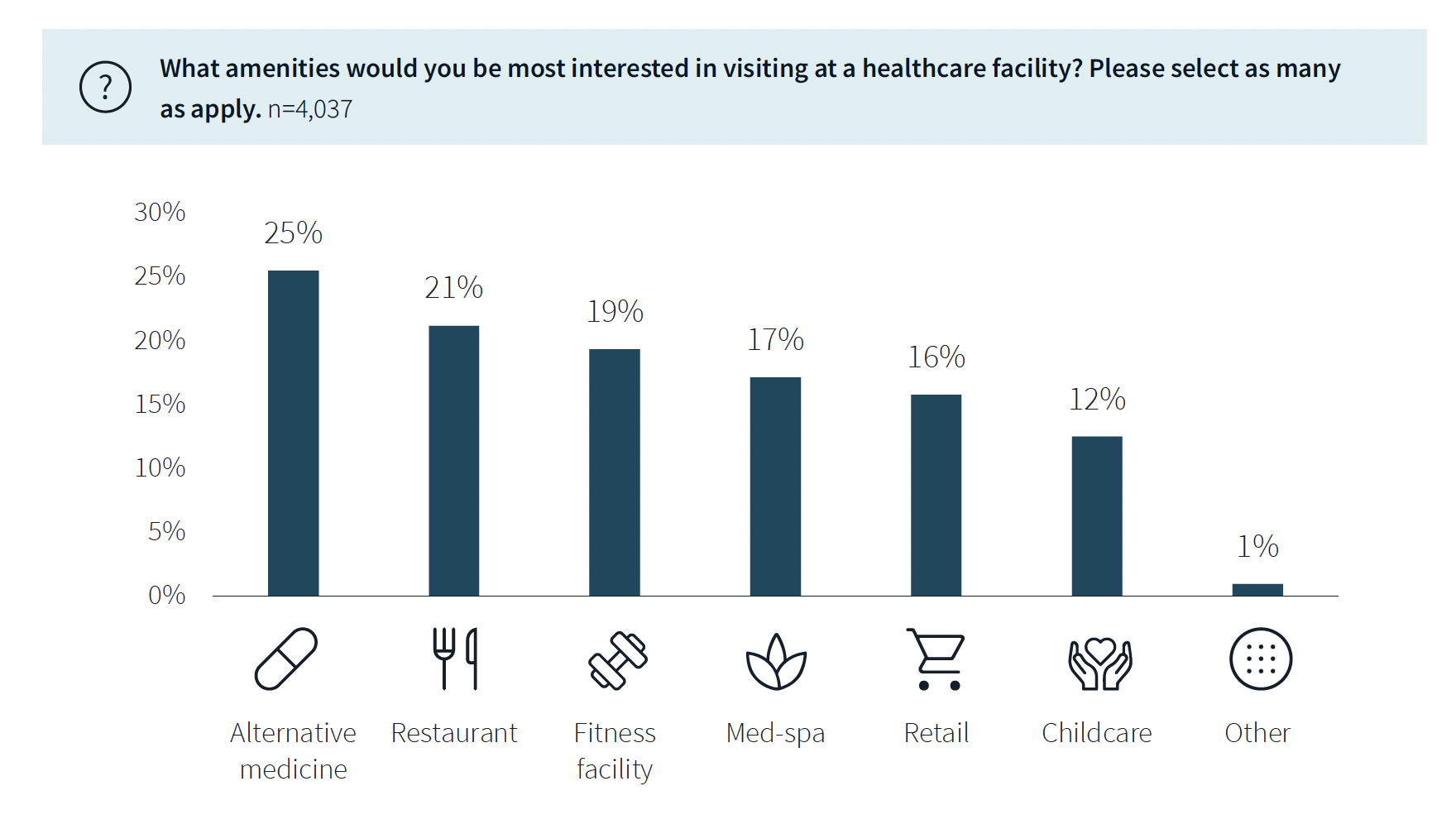
While not a decision-making factor, amenities do attract some patients. Among the survey’s respondents, 63% said they would be interested in visiting a healthcare facility with an additional amenity, such as alternative medicine, a restaurant, fitness center, or spa. (This inclination was more evident among younger respondents.)
The overall quality of facilities, including the comfort of their waiting rooms, can impact a patient’s choice, especially for inpatient, urgent, and emergency care. The survey also found that urban locations have lower favorability rankings for their facilities, signaling room for improvement. (Just under half—48%—of respondents live in the suburbs.)
Related Stories
| May 5, 2011
Hospitals launch quiet campaigns to drown out noise of modern medicine
Worldwide, sound levels inside hospitals average 72 decibels during the day and 60 decibels at night, which far exceeds the standard of 40 decibels or less, set by the World Health Organization. The culprit: modern medicine. In response, hospitals throughout Illinois and the U.S. are launching "quiet campaigns" that include eliminating intercom paging, replacing metal trash cans, installing sound-absorbing flooring and paneling, and dimming lights at night to remind staff to keep their voices down.
| Apr 14, 2011
USGBC debuts LEED for Healthcare
The U.S. Green Building Council (USGBC) introduces its latest green building rating system, LEED for Healthcare. The rating system guides the design and construction of both new buildings and major renovations of existing buildings, and can be applied to inpatient, outpatient and licensed long-term care facilities, medical offices, assisted living facilities and medical education and research centers.
| Apr 13, 2011
Virginia hospital’s prescription for green construction: LEED Gold
Rockingham Memorial Hospital in Harrisonburg, Va., is the commonwealth’s first inpatient healthcare facility to earn LEED Gold. The 630,000-sf facility was designed by Earl Swensson Associates, with commissioning consultant SSRCx, both of Nashville.
| Apr 12, 2011
Mental hospital in Boston redeveloped as healthcare complex
An abandoned state mental health facility in Boston’s prestigious Longwood Medical Area is being transformed into the Mass Mental Health Center, a four-building mixed-use complex that includes a mental health day hospital, a clinical and office building, a medical research facility for Brigham and Women’s Hospital, and a residential facility.
| Mar 17, 2011
Perkins Eastman launches The Green House prototype design package
Design and architecture firm Perkins Eastman is pleased to join The Green House project and NCB Capital Impact in announcing the launch of The Green House Prototype Design Package. The Prototype will help providers develop small home senior living communities with greater efficiency and cost savings—all to the standards of care developed by The Green House project.
| Mar 14, 2011
Renowned sustainable architect Charles D. Knight to lead Cannon Design’s Phoenix office
Cannon Design is pleased to announce that Charles D. Knight, AIA, CID, LEED AP, has joined the firm as principal. Knight will serve as the leader of the Phoenix office with a focus on advancing the firm’s healthcare practice. Knight brings over 25 years of experience and is an internationally recognized architect who has won numerous awards for his unique contributions to the sustainable and humanistic design of healthcare facilities.
| Mar 11, 2011
Renovation energizes retirement community in Massachusetts
The 12-year-old Edgewood Retirement Community in Andover, Mass., underwent a major 40,000-sf expansion and renovation that added 60 patient care beds in the long-term care unit, a new 17,000-sf, 40-bed cognitive impairment unit, and an 80-seat informal dining bistro.
| Mar 11, 2011
Research facility added to Texas Medical Center
Situated on the Texas Medical Center’s North Campus in Houston, the new Methodist Hospital Research Institute is a 12-story, 440,000-sf facility dedicated to translational research. Designed by New York City-based Kohn Pedersen Fox, with healthcare, science, and technology firm WHR Architects, Houston, the building has open, flexible labs, offices, and amenities for use by 90 principal investigators and 800 post-doc trainees and staff.
| Mar 11, 2011
Mixed-income retirement community in Maryland based on holistic care
The Green House Residences at Stadium Place in Waverly, Md., is a five-story, 40,600-sf, mixed-income retirement community based on a holistic continuum of care concept developed by Dr. Bill Thomas. Each of the four residential floors houses a self-contained home for 12 residents that includes 12 bedrooms/baths organized around a common living/social area called the “hearth,” which includes a kitchen, living room with fireplace, and dining area.