“Innovation” was the byword as 175 healthcare designers gathered in Chicago for the American College of Healthcare Architects/AIA Academy of Architecture for Health Summer Leadership Summit.
Experts from Kaiser Permanente, Cleveland Clinic, Mayo Clinic, Massachusetts General Hospital, and other healthcare institutions and think tanks described various models they’re using to spur innovation and improve the quality of care for their patients.
That’s a topic of mounting importance under the Affordable Care Act, which can penalize a hospital with a poor record of patient satisfaction and outcomes.
KAISER PERMANENTE. Jennifer Liebermann, Co-founder of Kaiser Permanente’s 37,000-sf Garfield Innovation Center, described a typical problem such in-house innovation facilities tackle: how to reduce medication errors. “Nurses get interrupted all the time when they’re trying to give patients their meds,” she said. That leads to medication errors and injury to patients.
HOW TO DESIGN A HEALTHCARE INNOVATION CENTER
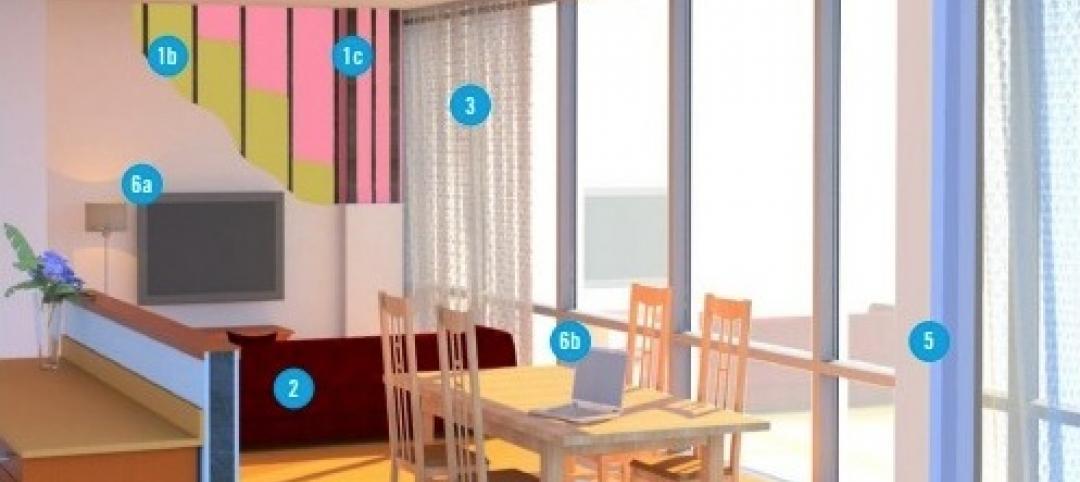
Larry Stofko, EVP of the Innovation Institute, provided ACHA/AAH summiteers with advice on designing physical spaces to enable innovation:
1. Make the space flexible, with movable walls and furnishings.
2. Make it inspiring, with whimsical artwork and “creative” colors (orange and blue seem to work best).
3. Make it collaborative, with lots of whiteboards, wall space, and glass to write on.
4. Make it social, with a working kitchen, comfy couches, springboard chairs.
5. Make it hard-working, by providing the right tools and hardware (e.g., 3D printers).
6. Make sure it reflects the institution’s culture and brand.
7. Provide a dedicated showcase to display your innovation successes.
The Garfield Center team tried several ideas, even something that looked like a hazmat suit (“We tested it on nurses, and they said they’d never wear that thing,” said Liebermann). The solution: a bright yellow sash that the nurse wears over her shoulder when dispensing prescriptions.
“That sash lets everyone know, ‘Don’t interrupt me, I’m dispensing meds,’” said Liebermann. A simple and inexpensive solution, but so effective that it’s being rolled out through the entire 32-hospital Kaiser Permanente system.
“We borrow ideas from other healthcare organizations, but some of our most powerful inspiration comes from outside healthcare,” said Liebermann. KP is working with Walmart on telemedicine and with NASA on improving safety in operating rooms. “NASA has a lot of experience with its people working in tight spaces,” she said.
CLEVELAND CLINIC is an institution with a long history of innovation in healthcare—2,600 patent applications, 450 royalty licenses, 71 spinoffs, $799 million in equity investments, according to Brian Kolonick, General Manager of Cleveland Clinic Innovations’ Global Healthcare Innovations Alliance. The alliance includes MedStar Health, North Shore–LIJ, Promedica, the University of Notre Dame, and Marshfield Clinic.
Half (50%) of the clinic’s inventions have been medical devices, along with IT solutions (23%) and therapeutic/diagnostic systems (22%). The remaining 5% were healthcare delivery solutions. “Delivery solutions are our secret sauce,” said Kolonick. Cleveland Clinic excels at coming up with new ways to improve patient outcomes and then outsourcing those capabilities to other institutions.
Cleveland Clinic is not modest about collaborating with the private sector and government agencies. It’s working with NASA Glenn Research Center to see how lessons from space medicine can be applied to terrestrial healthcare. They’re consulting with Parker Hannifan (“They know a lot about tubes, and we use a lot of tubes in healthcare,” said Kolonick) and Lubrizol, for its expertise in polymers.
“We’re also involved with Cox Communications, to see how they can help us work with patients from inside the home, or via healthcare pods at the grocery store,” he said.
MAYO CLINIC’s Center for Innovation was founded in 2008. “We’re a shared service for innovation across Mayo,” said Barbara Spurrier, MHA, CMPE, the CFI’s Administrative Director. Its staff of 60 includes scientists, designers, programmers, analysts, bioethicists, nurses, and lawyers.
The CFI has 47 projects in the works, most of which have to be completed in 12 months. “There are a lot of things that don’t work out,” Spurrier said. “Sometimes we get all the way to a prototype and it doesn’t work, and we have to put it on the shelf.”
Mayo is looking at developing smartphone apps, such as one that teenage asthma patients could use to monitor their condition without having to go to the clinic.
Video medical visits, perhaps via Skype, are of keen interest to Mayo, especially for use with older patients. “How can we help seniors thrive in place?” asked Spurrier. “We know that 85% of them can get their care at home. What conditions need to be in place so that we can serve them right in their homes?”
“The Garage” is another Mayo innovation initiative—an incubator for products and services with commercialization potential. There’s also CoDE, which provides as much as $50,000 each to up to 10 teams a year for what Spurrier called “open innovation.” Mayo’s “Transform” international symposium recently attracted 850 innovators from 16 countries.
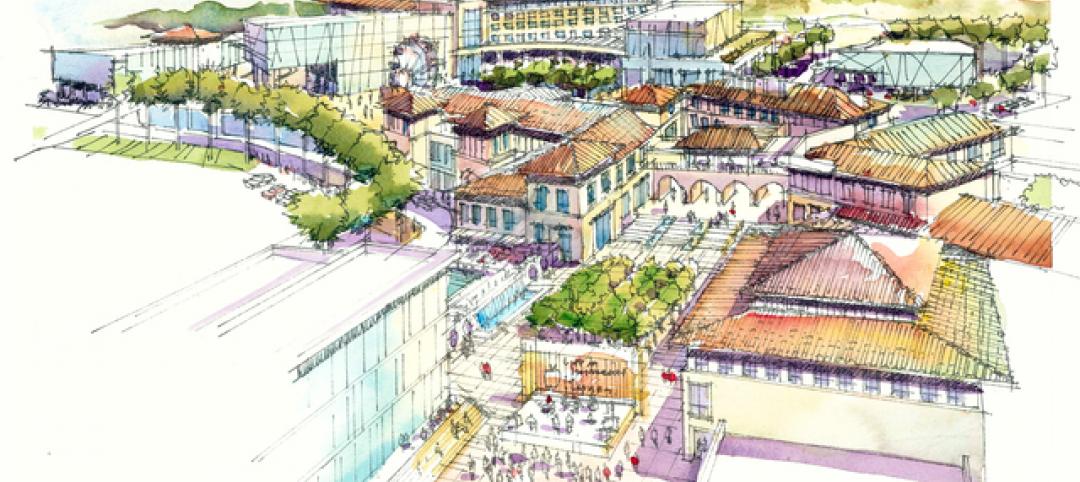
Mayo’s newest project: the 7,000-sf Well Living Lab, in collaboration with its home city of Rochester, Minn. “We’ll be looking at the intersection of medical and scientific research as related to the built environment,” said Spurrier.
MASS GENERAL. James A. Gordon, MD, MPA, Director of the Learning Laboratory at Massachusetts General Hospital and the Gilbert Program in Medical Simulation at Harvard Medical School, emphasized the need for simulation tools and labs at teaching hospitals. He said simulation training was crucial to improving patient safety and accelerating and assuring physician expertise.
“In medicine, every day is game day,” said Gordon, an emergency medicine specialist. To his fellow physicians, he posed this rhetorical question: “Can you continue to maintain your standards without allocating time for being offline to train?” Gordon didn’t say so outright, but it was clear he didn’t think so.
Related Stories
| Oct 30, 2014
CannonDesign releases guide for specifying flooring in healthcare settings
The new report, "Flooring Applications in Healthcare Settings," compares and contrasts different flooring types in the context of parameters such as health and safety impact, design and operational issues, environmental considerations, economics, and product options.
| Oct 30, 2014
Perkins Eastman and Lee, Burkhart, Liu to merge practices
The merger will significantly build upon the established practices—particularly healthcare—of both firms and diversify their combined expertise, particularly on the West Coast.
| Oct 21, 2014
Passive House concept gains momentum in apartment design
Passive House, an ultra-efficient building standard that originated in Germany, has been used for single-family homes since its inception in 1990. Only recently has the concept made its way into the U.S. commercial buildings market.
| Oct 21, 2014
Hartford Hospital plans $150 million expansion for Bone and Joint Institute
The bright-white structures will feature a curvilinear form, mimicking bones and ligament.
| Oct 16, 2014
Perkins+Will white paper examines alternatives to flame retardant building materials
The white paper includes a list of 193 flame retardants, including 29 discovered in building and household products, 50 found in the indoor environment, and 33 in human blood, milk, and tissues.
| Oct 15, 2014
Harvard launches ‘design-centric’ center for green buildings and cities
The impetus behind Harvard's Center for Green Buildings and Cities is what the design school’s dean, Mohsen Mostafavi, describes as a “rapidly urbanizing global economy,” in which cities are building new structures “on a massive scale.”
| Oct 13, 2014
Debunking the 5 myths of health data and sustainable design
The path to more extensive use of health data in green building is blocked by certain myths that have to be debunked before such data can be successfully incorporated into the project delivery process.
| Oct 12, 2014
AIA 2030 commitment: Five years on, are we any closer to net-zero?
This year marks the fifth anniversary of the American Institute of Architects’ effort to have architecture firms voluntarily pledge net-zero energy design for all their buildings by 2030.
| Oct 8, 2014
Massive ‘healthcare village’ in Nevada touted as world’s largest healthcare project
The $1.2 billion Union Village project is expected to create 12,000 permanent jobs when completed by 2024.
| Oct 3, 2014
Designing for women's health: Helping patients survive and thrive
In their quest for total wellness, women today are more savvy healthcare consumers than ever before. They expect personalized, top-notch clinical care with seamless coordination at a reasonable cost, and in a convenient location. Is that too much to ask?