A recent poll of healthcare providers found that 85% agree that most patients will not require an in-person physician evaluation by 2021. Virtual doctor visits will be common, smartphones and wearable sensors will be used widely to record a patient’s health information, and patients will have greater access to self-serving their health needs via technology equipped unmanned kiosks.
These are some of the predictions from the Mortenson Leadership Series Healthcare Study, the construction firm’s fourth in the last six years. The study is based on a poll of more than 900 healthcare professionals, facilities leaders, and architects who support them, conducted during last year’s ASHE Planning, Design, and Construction Summit.
While most of the study’s findings weren’t surprising, they confirm trends about Millennials’ healthcare expectations, how and where healthcare institutions will be investing, the role of technology in healthcare, and what roadblocks might lie ahead for project management.

Millennials' preferences for how they receive healthcare are having a major impact on how health systems are investing. Image: Mortenson
One thing is certain: patients are taking more ownership of their health. Eighty-three percent of the healthcare providers polled observe that patients are far more willing these days to shop for lower-cost care options. By 2021, 85% predict that providers will screen patients first to guide them to the appropriate treatment. And that won’t necessarily be toward a medical office or clinic.
One of the biggest disparities between the 2018 and 2015 surveys was the responses to the question about how common virtual doctors would be in three years’ time. Last year, 88% responded to this question affirmatively, compared to 63% in 2015. And 85% in the 2018 surveyed participants thought that most patients don’t require an in-person physician evaluation, versus 49% in 2015.
As one 2018 respondent noted, “Millennials expect immediate access. This access will drive how we design facilities as well as garner a new age of telehealth.” Two-fifths of healthcare providers and architects mentioned that virtual telemedicine and self-service treatments would be typical delivery care within the next decade, with much less reliance on physical structures to deliver goods and services.
Healthcare facilities managers say their institutions must become leaner to grapple with insufficient project resources. Many see opportunities in reducing waste and energy consumption. Image: Mortenson
More than two-fifths (44%) of architects polled also said that Millennials’ expectations about the need for more integration and utilization of technology is impacting healthcare and its facilities, followed by 22% who cited the demand for convenience and virtual care. “Less acute, more ambulatory. Less invasive procedures. More virtual … diagnosis and treatments,” stated one respondent.
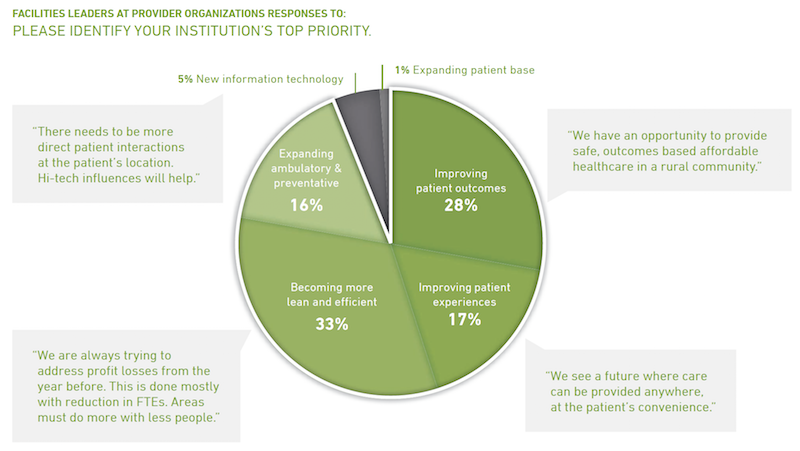
Two thirds of facilities leaders polled said that their institutions would invest more over the next two to three years. But 35% added that their biggest challenge continues to be insufficient money and resources (including receiving adequate payments for services rendered), followed by “growing pains” (18%) and project delivery (17%).
Nearly half of facilities leaders polled say their healthcare systems continue to invest in clinics, ambulatory care centers, and medical offices. Image: Mortenson
Nearly all of the facilities leaders see significant opportunities to eliminate waste and reduce energy use.
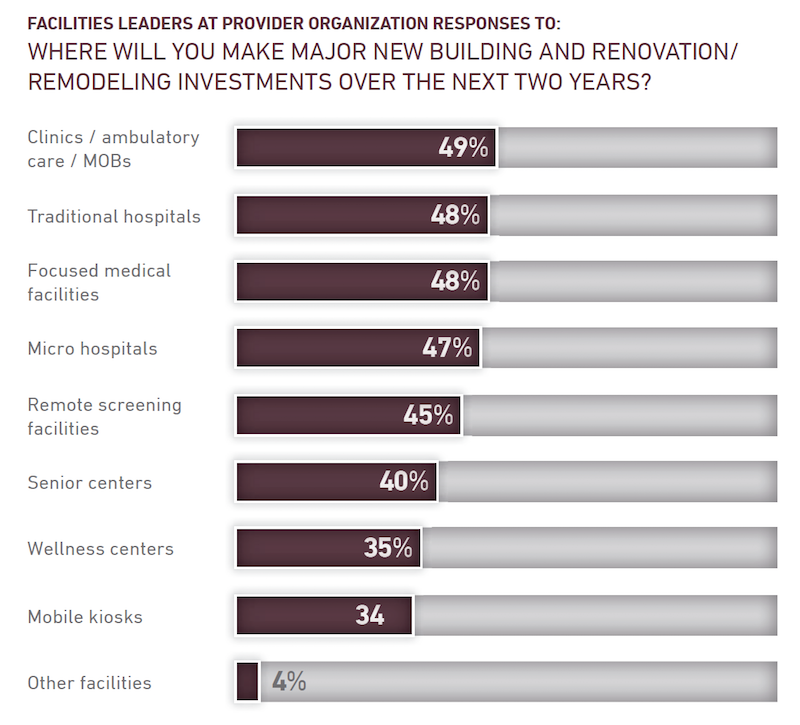
Despite all of speculation about virtual care expressed in the study, 49% of facilities leaders said their institutions would be making major investments in clinics, ambulatory care, and MOBs, followed by traditional hospitals and focused medical facilities (48% each), microhospitals (47%), and remote screening facilities (45%).
The respondents were evenly split about how much their institutions might spend over the next two years, with 33% each projecting moderate, substantial, or flat growth.
The study includes a section about the Affordable Care Act. Fewer respondents in 2018 than in 2015 thought the legislation had done enough to address the country’s long-term healthcare needs. And between 94% and 97% of those polled last year said that the Act still needed “significant changes or revisions,” had created uncertainty for their institutions, and had challenged their organization’s near-term financial condition.
Related Stories
Daylighting | Aug 18, 2022
Lisa Heschong on 'Thermal and Visual Delight in Architecture'
Lisa Heschong, FIES, discusses her books, "Thermal Delight in Architecture" and "Visual Delight in Architecture," with BD+C's Rob Cassidy.
| Aug 16, 2022
Cedars-Sinai Urgent Care Clinic’s high design for urgent care
The new Cedars-Sinai Los Feliz Urgent Care Clinic in Los Angeles plays against type, offering a stylized design to what are typically mundane, utilitarian buildings.
| Aug 15, 2022
IF you build it, will they come? The problem of staff respite in healthcare facilities
Architects and designers have long argued for the value of respite spaces in healthcare facilities.
AEC Tech | Aug 8, 2022
The technology balancing act
As our world reopens from COVID isolation, we are entering back into undefined territory – a form of hybrid existence.
| Aug 3, 2022
Designing learning environments to support the future of equitable health care
While the shortage of rural health care practitioners was a concern before the COVID-19 pandemic, the public health crisis has highlighted the importance of health equity in the United States and the desperate need for practitioners help meet the needs of patients in vulnerable rural communities.
Healthcare Facilities | Aug 1, 2022
New Phoenix VA outpatient clinic is one of the largest veteran care facilities in the U.S.
The new Phoenix 32nd Street VA Clinic, spanning roughly 275,000 sf over 15 acres, is one of the largest veteran care facilities in the U.S.
Building Team | Jul 12, 2022
10 resource reduction measures for more efficient and sustainable biopharma facilities
Resource reduction measures are solutions that can lead to lifecycle energy and cost savings for a favorable return on investment while simultaneously improving resiliency and promoting health and wellness in your facility.
Healthcare Facilities | Jun 22, 2022
Arizona State University’s Health Futures Center: A new home for medical tech innovation
In Phoenix, the Arizona State University (ASU) has constructed its Health Futures Center—expanding the school’s impact as a research institution emphasizing medical technology acceleration and innovation, entrepreneurship, and healthcare education.
Healthcare Facilities | Jun 20, 2022
Is telehealth finally mainstream?
After more than a century of development, telehealth has become a standard alternative for many types of care.
Codes and Standards | Jun 14, 2022
Hospitals’ fossil fuel use trending downward, but electricity use isn’t declining as much
The 2021 Hospital Energy and Water Benchmarking Survey by Grumman|Butkus Associates found that U.S. hospitals’ use of fossil fuels is declining since the inception of the annual survey 25 years ago, but electricity use is dipping more slowly.

















