A recent poll of healthcare providers found that 85% agree that most patients will not require an in-person physician evaluation by 2021. Virtual doctor visits will be common, smartphones and wearable sensors will be used widely to record a patient’s health information, and patients will have greater access to self-serving their health needs via technology equipped unmanned kiosks.
These are some of the predictions from the Mortenson Leadership Series Healthcare Study, the construction firm’s fourth in the last six years. The study is based on a poll of more than 900 healthcare professionals, facilities leaders, and architects who support them, conducted during last year’s ASHE Planning, Design, and Construction Summit.
While most of the study’s findings weren’t surprising, they confirm trends about Millennials’ healthcare expectations, how and where healthcare institutions will be investing, the role of technology in healthcare, and what roadblocks might lie ahead for project management.

Millennials' preferences for how they receive healthcare are having a major impact on how health systems are investing. Image: Mortenson
One thing is certain: patients are taking more ownership of their health. Eighty-three percent of the healthcare providers polled observe that patients are far more willing these days to shop for lower-cost care options. By 2021, 85% predict that providers will screen patients first to guide them to the appropriate treatment. And that won’t necessarily be toward a medical office or clinic.
One of the biggest disparities between the 2018 and 2015 surveys was the responses to the question about how common virtual doctors would be in three years’ time. Last year, 88% responded to this question affirmatively, compared to 63% in 2015. And 85% in the 2018 surveyed participants thought that most patients don’t require an in-person physician evaluation, versus 49% in 2015.
As one 2018 respondent noted, “Millennials expect immediate access. This access will drive how we design facilities as well as garner a new age of telehealth.” Two-fifths of healthcare providers and architects mentioned that virtual telemedicine and self-service treatments would be typical delivery care within the next decade, with much less reliance on physical structures to deliver goods and services.
Healthcare facilities managers say their institutions must become leaner to grapple with insufficient project resources. Many see opportunities in reducing waste and energy consumption. Image: Mortenson
More than two-fifths (44%) of architects polled also said that Millennials’ expectations about the need for more integration and utilization of technology is impacting healthcare and its facilities, followed by 22% who cited the demand for convenience and virtual care. “Less acute, more ambulatory. Less invasive procedures. More virtual … diagnosis and treatments,” stated one respondent.
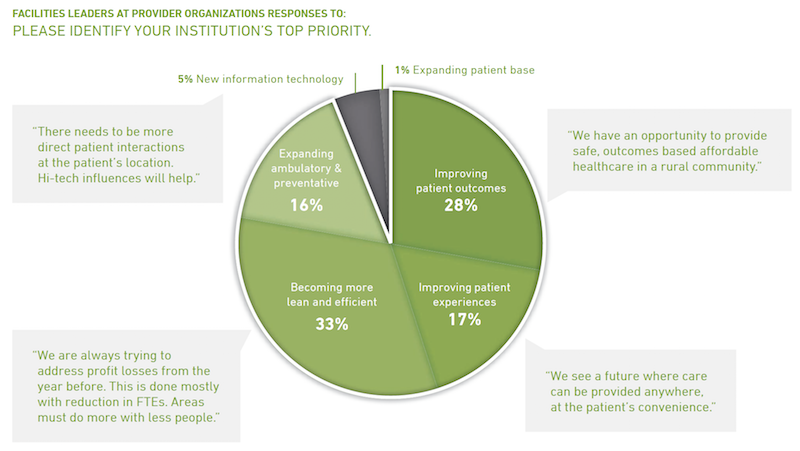
Two thirds of facilities leaders polled said that their institutions would invest more over the next two to three years. But 35% added that their biggest challenge continues to be insufficient money and resources (including receiving adequate payments for services rendered), followed by “growing pains” (18%) and project delivery (17%).
Nearly half of facilities leaders polled say their healthcare systems continue to invest in clinics, ambulatory care centers, and medical offices. Image: Mortenson
Nearly all of the facilities leaders see significant opportunities to eliminate waste and reduce energy use.
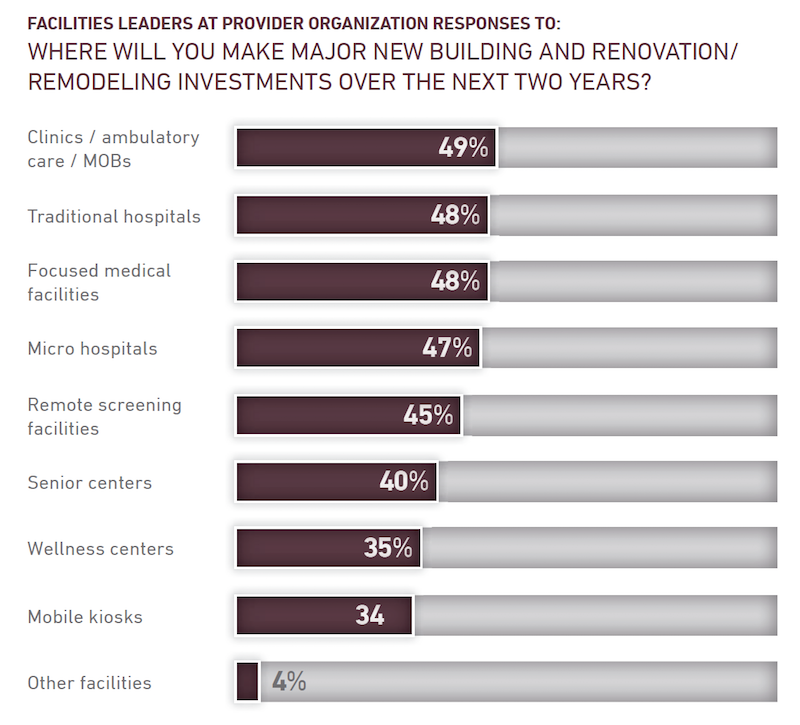
Despite all of speculation about virtual care expressed in the study, 49% of facilities leaders said their institutions would be making major investments in clinics, ambulatory care, and MOBs, followed by traditional hospitals and focused medical facilities (48% each), microhospitals (47%), and remote screening facilities (45%).
The respondents were evenly split about how much their institutions might spend over the next two years, with 33% each projecting moderate, substantial, or flat growth.
The study includes a section about the Affordable Care Act. Fewer respondents in 2018 than in 2015 thought the legislation had done enough to address the country’s long-term healthcare needs. And between 94% and 97% of those polled last year said that the Act still needed “significant changes or revisions,” had created uncertainty for their institutions, and had challenged their organization’s near-term financial condition.
Related Stories
| Mar 21, 2012
Iowa’s Mercy Medical Center’s new Emergency Department constructed using Lean design
New Emergency Department features a "racetrack" design with a central nurses' station encircled by 19 private patient examination rooms and 2 trauma treatment rooms.
| Mar 19, 2012
HKS Selected for Baylor Medical Center at Waxahachie
Baylor Medical Center at Waxahachiewill incorporate advanced technology including telemedicine, digital imaging, remote patient monitoring, electronic medical records and computer patient records.
| Mar 14, 2012
Tsoi/Kobus and Centerbrook to design Jackson Laboratory facility in Farmington, Conn.
Building will house research into personalized, gene-based cancer screening and treatment.
| Mar 6, 2012
Country’s first Green House home for veterans completed
Residences at VA Danville to provide community-centered housing for military veterans.
| Mar 1, 2012
7 keys to ‘Highest value, lowest cost’ for healthcare construction
The healthcare design and construction picture has been muddied by uncertainty over the new healthcare law. Hospital systems are in a bind, not knowing what levels of reimbursement to expect. Building Teams serving this sector will have to work even harder to meet growing client demands.
| Feb 29, 2012
Construction begins on Keller Army Community Hospital addition
The 51,000 square foot addition will become the home for optometry, ophthalmology, physical therapy, and orthopedics clinics, as well as provide TRICARE office space.
| Feb 29, 2012
Shepley Bulfinch selected to design new Children’s Hospital of Buffalo
The firm was selected because of their past experience in designing clinically complex facilities that emphasize patient- and family-centered care and operational efficiency as well as distinctive architectural forms for many other children's and women's hospitals.
| Feb 28, 2012
More than 1,000 have earned EDAC certification since 2009
Milestone achieved as evidence-based design becomes a top 2012 strategy for healthcare organizations.
| Feb 28, 2012
McCarthy completes second phase of San Diego’s Scripps Hospital
Representing the second phase of a four-phased, $41.3 million expansion and remodeling project, the new addition doubles the size of the existing emergency department and trauma center to encompass a combined 27,000 square feet of space.
















